How would you treat this elderly male with one day of chest pain and shortness of breath?
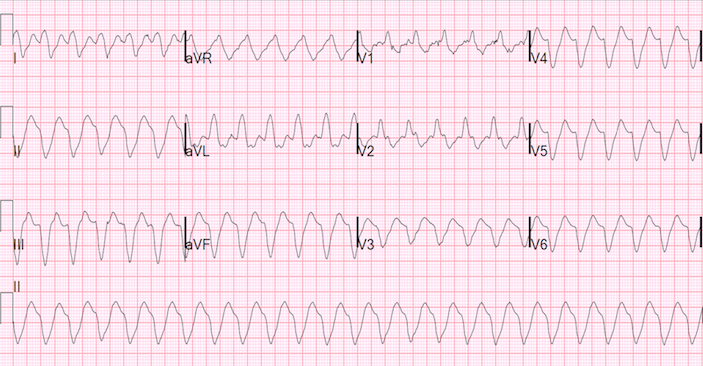
An elderly male who missed dialysis presented to the emergency department complaining of one day of chest pain and shortness of breath at rest. Upon arrival to the ED, he was awake, well perfused and neurologically intact, and this ECG was obtained (Image 1 above).
This is a very wide complex tachycardia, with a sine wave morphology at a rate of about 160, and a QRS duration of about 220 ms. There are no visible P-waves. Sinus tachycardia with hyperkalemia by itself can have exactly this morphology (sine wave), but should not be so fast unless the patient is critically ill. P-waves flatten and disappear in hyperkalemia and so might be invisible even though the sinus node is driving the rhythm. On the other hand, ventricular tachycardia is fast – but rarely has such a sine wave morphology with such a super-wide QRS. Thus, this is very likely ventricular tachycardia in the presence of hyperkalemia, especially as VT is a common complication of severe hyperkalemia.
But what if this is supraventricular tachycardia with aberrancy, and superimposed hyperkalemia?
Again, arguing against isolated hyperkalemia is the very fast heart rate. Hyperkalemia with extreme tachycardia may be present without VT in severely ill patients. However, our patient is not extremely ill and it would be more common to have a lower heart rate.
It would be appropriate to treat for both dysrhythmia and hyperkalemia, using cardioversion and Calcium and Potassium shifting therapy.
For stable ventricular tachycardia, the typical method of cardioversion recommended for providers in general is chemical. However, electrical cardioversion is safer if you are skilled at procedural sedation, as most emergency physicians are. Chemical cardioversion (with the exception of adenosine) carries a high risk of hypotension, prolonged QT, and pro-arrhythmia. Electrical cardioversion is brief and has no lasting adverse effects.
*********
The ED providers went on to give the patient calcium gluconate, and IV insulin and dextrose to shift the patient’s (presumed) hyperkalemia. As they were doing this, the potassium returned at 7.4 mEq/L.
The next ECG at 19 minutes later looked like this (image 2 below). The rate remains very fast, but the QRS width is now much narrower at about 180 ms. It is still very wide and strongly suggests ventricular tachycardia. However, supraventricular tachycardia with aberrancy might also be very wide in the setting of hyperkalemia. Notice that there is a right bundle branch block (RBBB) morphology (rR’-wave in V1 and deep wide S-wave in V5 and V6. There is also extreme left axis deviation with small r-waves in inferior leads followed by a large S-wave, and a small q-wave in aVL with a large R-wave; this is a left anterior fascicular block (LAFB) morphology.
Thus, this could be a supraventricular tachycardia (SVT) with aberrancy (in this case the aberrancy is RBBB and LAFB). It might respond to adenosine, which is not contra-indicated in ventricular tachycardia.
A third ECG at 34 minutes looked identical. ECG 3 is not shown.
Treatment of hyperkalemia will shorten the QRS duration of VT or of SVT with aberrancy.
As emergent dialysis was being prepared, the patient’s mental status began to decline and the decision was made to intubate and cardiovert the patient. After intubation he was cardioverted (synchronized, 100J) with a single shock.
This was his subsequent ECG (image 3 below).
There is now sinus rhythm at a rate of about 100. The successful conversion definitely confirms that the previous fast rhythm was indeed a re-entrant shockable rhythm, VT vs. SVT with aberrancy. There is RBBB and a QRS duration of 175 ms (long for RBBB, but typical for RBBB with hyperkalemia). There is also LAFB.
So the QRS morphology in sinus is the same as in tachycardia, strongly suggesting that the previous rhythm was indeed SVT with aberrancy!
Comment: It would have probably worked very well to convert earlier. And it would have been useful to try adenosine first. It would be safe, could be effective from a prospective point of view, and looking retrospectively, probably would have been effective. If electrical cardioversion were necessary, I would not use propofol for sedation as it could cause catastrophic hypotension, but would give a small dose of ketamine. I believe that intubation could have been avoided if cardioversion with ketamine had been done early.
Of note, the patient later was shown to have a baseline RBBB/LAFB morphology, but, his QRS was not typically this wide. RBBB alone should have a QRS duration less than 170 ms.
Later, after more decline in the potassium, a 5th ECG was recorded with a QRS duration of 157 ms.
The patient went on to emergent dialysis, was extubated later that day. He was discharged and is doing well.
TEACHING POINTS
- Any wide QRS may be due to hyperkalemia.
- Baseline RBBB or LBBB usually has a QRS duration < 170 ms. Any longer should raise your suspicion of hyperkalemia even higher.
- In the presence of hyperkalemia, SVT with aberrancy can look very wide and mimic ventriclar tachycardia.
- Adenosine is not contraindicated in ventricular tachycardia. It is only contraindicated in atrial fibrillation with WPW, in which case there should be 3 major findings: 1) irregulary irregular rhythm 2) multiform QRS complexes and 3) some extremely short R-R intervals (shortest RR interval always < 250 ms).
- When circulation is the primary perturbation, attention to airway and breathing does not necessarily come before circulation. This patient’s airway only became compromised because of progressive shock with altered mental status; managing his perfusion earlier would have obviated the need for airway management.











2 Comments
I think the diagnosis of SVT with aberrant conduction is obvious from the first two EKGs, as P waves can be seen both in V1 (EKG 1 & 2) and frontal lead I (EKG 2). The very short PR interval is confirmed when the patient returns to sinus rhythm in EKG #3.
With retrospective goggles, I agree with you David Nunley.