Start with three quick bedside ultrasounds and you might avoid an unnecessary IV push
An 11-year-old boy is brought to your emergency department following a few hours of persistent vomiting, irritability and decreasing activity. His mother also reports about two days of fever, decreased appetite and nasal stuffiness.
On initial evaluation, his vital signs include a heart rate of 128 beats/minute, blood pressure of 82/64 mmHg, respirations of 24 breaths/minute and temperature of 101.50F. Pulse oximetry reveals 98% saturation on room air while capillary refill time is approximately 5 seconds. His activity is reduced and skin mottling is evident. His rate and depth of breathing is, however, only slightly increased and his lungs are clear.
It is apparent that your patient is in shock and your staff has already started working on intravenous access. One of your most pediatric-experienced nurses asks whether you want 20 cc/kg of normal saline to be pushed as quickly as possible.
At this point, the little voice that speaks to most emergency physicians interjects, “Are you sure this is not cardiogenic shock? Could this be the one?”
In a previous issue of Soundings, we discussed the case of a 7-year-old child where a strategic approach to ultrasound assisted in diagnosis and resuscitation subsequent to major blunt trauma. In this issue, we will review a systematized approach to the more common presentation of undifferentiated shock.
Your response to the nurse is, appropriately, “let me take a look first.”
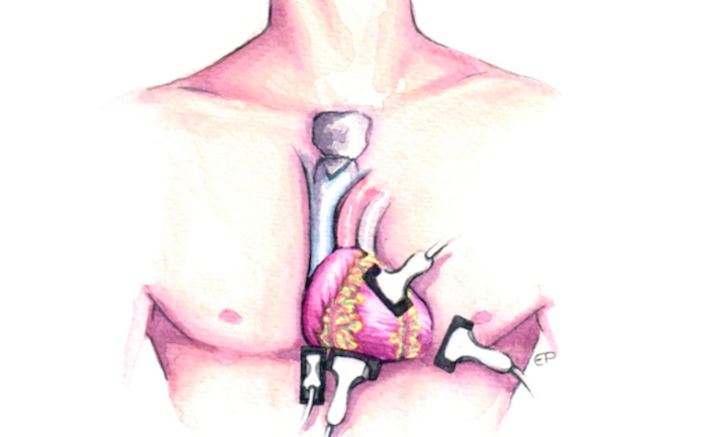
 You begin your ultrasound evaluation using a curvilinear probe and, to the surprise of everyone in the room, including yourself, a large pericardial effusion is readily apparent (Figure 1). Your patient’s cardiac morphology appears otherwise normal. Resisting the temptation to marvel at this uncommon pediatric sonographic finding, you quickly move your probe to a sagittal subcostal orientation in order to obtain a long-axis view of the inferior vena cava (IVC). The child’s IVC is large and demonstrates only minimal fluctuation in size during the respiratory cycle (Figure 2). Your nursing staff continues to expectantly await direction while a pericardiocentesis tray has appeared at the bedside.
You begin your ultrasound evaluation using a curvilinear probe and, to the surprise of everyone in the room, including yourself, a large pericardial effusion is readily apparent (Figure 1). Your patient’s cardiac morphology appears otherwise normal. Resisting the temptation to marvel at this uncommon pediatric sonographic finding, you quickly move your probe to a sagittal subcostal orientation in order to obtain a long-axis view of the inferior vena cava (IVC). The child’s IVC is large and demonstrates only minimal fluctuation in size during the respiratory cycle (Figure 2). Your nursing staff continues to expectantly await direction while a pericardiocentesis tray has appeared at the bedside.
 Your response is, appropriately, “I need to look at one more thing.”
Your response is, appropriately, “I need to look at one more thing.”
You have already identified a problem with the “pump” and the IVC – the “tank” – certainly appears full. You now need to evaluate the “pipes” that reside within the lung parenchyma.
You apply a linear probe to the chest wall and note persistently recurring horizontal lines visible at regular intervals below normally-shimmering pleura from which occasional comet tail artifacts nudge downward (Figure 3). These pulmonary A-lines are apparent in multiple lung segments. Very few vertical densities extending through the depth of assessed lung segments – B-lines – are appreciated during your quick overview. You are aware that pulmonary A-lines are a normal “default artifact” and are erased by the transmission of sound waves through parenchymal lung fluid. Therefore, your judgment is that cardiogenic pulmonary edema is not present; at least not yet. Meanwhile, your patient continues to be in shock.
 This is a quintessential example of an urgent resuscitation decision that is best-informed using bedside ultrasound. Although administering a fluid bolus in the face of a significant pericardial effusion seems counter-intuitive to your staff, you explain that the patient’s lungs are clear, his oxygenation is satisfactory, and that your lung ultrasound is reassuring. Moreover, you anticipate that careful administration of intravenous fluid will improve his perfusion, your first priority.
This is a quintessential example of an urgent resuscitation decision that is best-informed using bedside ultrasound. Although administering a fluid bolus in the face of a significant pericardial effusion seems counter-intuitive to your staff, you explain that the patient’s lungs are clear, his oxygenation is satisfactory, and that your lung ultrasound is reassuring. Moreover, you anticipate that careful administration of intravenous fluid will improve his perfusion, your first priority.
Following your provision of 10 milliliters per kilogram of normal saline (one-half the customary fluid bolus), your patient’s blood pressure increases to 100/60 mmHg while his capillary refill decreases to 3 seconds. Clinical and sonographic re-evaluation reveals no evidence of increased pulmonary interstitial fluid. You are now able to spend a little more time evaluating the pericardial effusion and your patient’s cardiopulmonary status. You utilize additional cardiac windows to more fully assess the magnitude, location and potential accessibility of the pericardial effusion as well as its effect on cardiorespiratory status (Figure 4). Your cardiologist arrives, reviews your videos, and agrees to observe as opposed to performing an immediate pericardiocentesis.
 You admit your patient to the cardiology service where he is treated with ibuprofen, rest, careful hydration and continuous cardiac monitoring. His perfusion improves, pericardiocentesis is not needed, and the pericardial effusion fully resolves shortly following discharge from the hospital.
You admit your patient to the cardiology service where he is treated with ibuprofen, rest, careful hydration and continuous cardiac monitoring. His perfusion improves, pericardiocentesis is not needed, and the pericardial effusion fully resolves shortly following discharge from the hospital.
Days later, your provision of an intravenous fluid bolus to a child with a substantial pericardial effusion is discussed during a case conference. You explain that intravenous fluid will not immediately enter the pericardial sac and produce critical tamponade. Moreover, increased intra-ventricular volume in the face of acute diastolic dysfunction can improve cardiac output and systemic perfusion to provide at least temporizing benefit during preparation for pericardiocentesis. In this case, it resulted in hemodynamic stability while time and appropriate treatment caused improvement of the pericardial effusion.
Pearls & Pitfalls For Using Ultrasound During the Assessment of the Unstable Child
- Beware the vomiting infant or child, particularly when unassociated with diarrhea. Vomiting is occasionally a non-specific manifestation of metabolic stress in children and should cause consideration of other possible conditions, some quite significant. Moreover, vomiting, by itself, is not an effective means of emptying the stomach (consider the disappearance of Syrup of Ipecac) and therefore is seldom the sole cause of profound or rapidly-developing dehydration. Advice? –Sound around.
- A systematic sonographic approach to undifferentiated pediatric shock is advisable. In children with cardiorespiratory and even neurologic compromise, ultrasound may rapidly provide unanticipated information that markedly changes resuscitation decisions. In our example, bedside ultrasound caused us to depart from our customarily aggressive “IV Push” fluid resuscitation of the febrile child suspected for septic/distributive shock.
- A simple, time-efficient and memorable approach to the unstable child begins with 3 ultrasound assessments. We begin in the subxiphoid position to assess cardiac contractility and for the possible presence of pericardial effusion. From this position, we quickly rotate the probe clockwise slightly less than 90 degrees to assess size and respiratory variation of the IVC. Most of the shocky children we evaluate have a vigorously contracting heart, no pericardial effusion, and a small IVC which varies considerably in size during the respiratory cycle. The third phase of our stability screening scan involves the rapid assessment of multiple lung segments where we usually note normal sliding pleura with occasional comet-tail artifact, multiple unattenuated A-lines, and very few B-lines. This initial assessment can be accomplished within 60 seconds and provides direction regarding fluid resuscitation, possible need for positive pressure ventilation and the use of inotropes and/or pressors.
- Scan further to screen for unanticipated causes of volume loss or obstruction to flow. Even when hypovolemic or distributive/septic shock appears to be the problem, a sonographic search for unusual conditions is suggested. Intravascular volume depletion may occur due to splenic sequestration, mononucleosis-associated splenic rupture, ectopic pregnancy, and unanticipated long bone fracture. Infant Intra-ventricular Hemorrhage (IVH) may cause considerable volume loss associated with an expansible cranium while occult pneumothorax can obstruct venous return and compromise cardiac output. Without ultrasound, the diagnosis of these and other unusual conditions are frequently delayed, risking increased morbidity and mortality.
- Stability Screening Scans may prove useful to a variety of practitioners. Rapid assessment teams, delivery room staff, paramedics, health care professionals supervising athletic events, providers-in-triage and those practicing medicine in austere settings may utilize ultrasound for point-of-care assessment. The availability of hand-held scanners may someday mimic the stethoscope and expedite specific remediable diagnoses and treatments.