What can bedside ultrasound tell you about this 10-month-old girl suffering from abdominal pain?
It is a ridiculously busy Saturday night in your emergency department, made worse by the extra hour associated with the “fall-back” due to the change from daylight savings to standard time. At about 0400, a 10-month-old female is brought to your ED by her parents for intermittent but intense episodes of crying that began about six hours ago. In addition, her parents report two episodes of vomiting. She is otherwise symptom-free, with no fever, diarrhea or respiratory illness.
On examination, the baby appears very tired but with intervening and discrete episodes of crying that appear to occur in response to pain. Another emesis occurs during your examination, with your observation that the content is slightly green in color. You order three-view abdominal radiography and, while waiting for the tech to arrive, prepare for a bedside ultrasound while nursing sets up for an intravenous line. One of your more experienced nurses wonders aloud whether you’ve forgotten to provide your “usual” small dose of fentanyl analgesia to facilitate abdominal ultrasound examination. You mention that this particular situation is likely not appendicitis – your usual reason – and that analgesia in this case might actually prove to be counter-productive.
The infant’s crying appears to be paroxysmal, more characteristic of visceral as opposed to somatic pain, and suggestive of entities such as bowel obstruction and nephrolithiasis. Although not all classic signs of intussusception are present, you mention that the majority of cases are incomplete, and initiate your pursuit of this diagnosis.
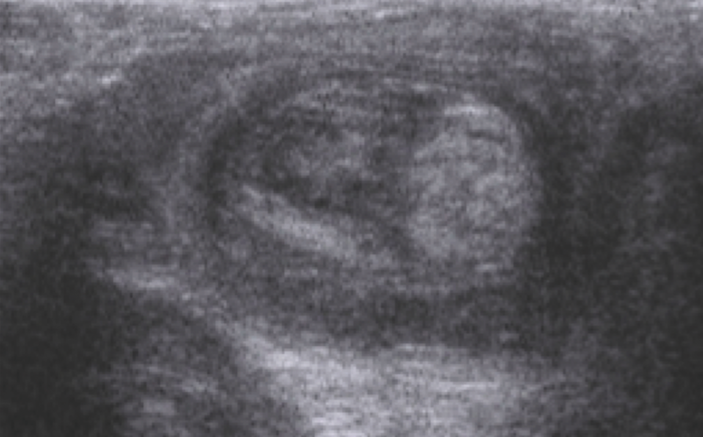
Using warmed gel and a linear high-frequency transducer; you begin insonating at the infant’s cecum, moving proximally toward the right upper quadrant, aligning the transducer in a transverse orientation to the colon. You notice a mass in the right upper quadrant anterior to a normal-appearing right kidney. A hypoechoic ring surrounds a heterogeneous and relatively echodense center (Figure 1 at top of screen). You believe these findings represent an intussuscipiens and intussusceptum, respectively. As you rotate your probe toward a long-axis view of the mass, you notice a “pseudo-kidney” appearance (Figure 2 below). Additional rotation brings the mass into a more pure long-axis alignment and reveals a “Y” shaped structure that resembles a characteristic “hayfork sign,” providing additional confirmation of intussusception (Figure 3 below). Plain abdominal radiographs obtained immediately following your bedside ultrasound are also worrisome for intussusception but, fortunately, reveal no evidence suggesting bowel wall perforation that would preclude attempted air enema reduction. You consult radiology and, in concert with your institution’s temporary shortage of ultrasound techs, you inquire as to whether the bedside images you have acquired and stored might be acceptable. The radiologist accesses your ultrasound images and plain abdominal radiographs from his home PACS connection and requests that the patient arrive in the fluoroscopy suite in approximately 15 minutes for attempted reduction. With the infant still crying, an air-enema is performed under fluoroscopic guidance and successfully reduces the intussusception. The infant subsequently relaxes, naps and appears well throughout a period of monitored post-reduction observation. No signs of perforation or recurrence are noted. He is discharged home with instructions for careful observation and recovers uneventfully.
 Figure 2. Pseudokidney sign of intussusception
Figure 2. Pseudokidney sign of intussusception
 Figure 3. Hayfork sign of intussusception
Figure 3. Hayfork sign of intussusception
As you debrief with your staff, you are asked again why you opted to not provide analgesia for a child in such obvious severe pain, particularly following your establishment of the diagnosis. You explain that most experienced radiologists find it safer when patients undergoing reduction are sufficiently awake to cry, scream and valsalva during the procedure (see Teaching Point 8). Although you’re not certain the staff is buying your explanation, it is clear they are relieved and more than a little impressed with the infant’s remarkable improvement.
Key Teaching Points
- The differential diagnosis of the so-called crying infant is extensive and includes numerous disparate entities. Although most causative conditions will resolve spontaneously and are not dangerous, considerable practitioner judgment is needed for those illnesses that may result in significant morbidity if left undetected. Point-of-Care Ultrasound can be utilized as an adjunct to a multisystem evaluation that can expedite the detection of potentially life-threatening pediatric illness.
- The differential diagnosis of bilious vomiting in infants and young children is also broad. A useful adage is that the younger the patient, the earlier the appearance of bile-staining, and the fewer associated systemic symptoms, the more likely the cause of vomiting is mechanical obstruction distal to the Ligament of Treitz. The absence of fever and the early onset of bilious emesis in this case should heighten one’s concern.
- Intussusception often serves as a “poster-child” for visceral pain. The discomfort associated is frequently intense and spasmodic with intervening periods of exhaustion that may resemble coma. The classic clinical triad of acute intussusception consists of paroxysmal abdominal pain, vomiting, and currant-jelly stools consisting of blood and mucus. However, this classic triad occurs in less than 25% of those ultimately diagnosed with the condition. Although a palpable, sausage-like, right upper quadrant mass is occasionally appreciable, its detection is undependable on physical exam and, therefore, not a sensitive indicator of the condition.
- Ultrasound assessment for intussusception began as a diagnostic alternative to barium or iodinated contrast enema. Initial ultrasound evaluation provides greater certainty of intussusception as opposed to similarly presenting colitis and diminishes the risk of pressure-induced perforation of friable and inflamed intestine in the latter condition. The use of diagnostic ultrasound has also decreased the number of children exposed to radiation associated with fluoroscopy. Ultrasound accuracy is excellent in the hands of an experienced sonographer with additional reports of rapid skill acquisition by trainees. Although fluoroscopically guided air enema remains the usual mode of reduction for visualized ileocolic intussusception, some centers have successfully employed ultrasound for visual confirmation of saline enema reduction, further decreasing the use of fluoroscopy and its attendant radiation exposure. Plain radiography continues to be well utilized when intussusception is a consideration and its “panoramic view” can provide the radiologist an overview of the situation prior to air enema. Noteworthy plain radiographic features include the following: (1) Distal bowel gas is often diminished or absent in the presence of intussusception due to global intestinal hyperperistalsis resulting from the obstruction. (2) Conversely, the use of a prone cross-table lateral x-ray, which positions the rectum as the highest point of the intestinal tract, provides some reassurance against intussusception if distal air is present. (3) A screening left lateral decubitus x-ray is also useful as a screening test as the presence of an entirely air-filled right colon similarly provides reasonable assurance against ileocolic intussusception.
- An intussusception typically measures between two and five centimeters in diameter and characteristically does not contain bowel gas, facilitating its identification with ultrasound. It often has a hypoechic rim, representing edematous bowel wall (the containing intussuscipiens). Concentric hypoechoic peripheral rings may also be noted. The contained hyperechoic/heterogeneous center (intussusceptum) consists of compressed and eccentrically positioned mesenteric fat, blood vessels and lymph nodes (Figure 4 below: The arrow head designates the circumfrential layers of the containing intussuscipiens while the arrow points to the hyperechoic eccentrically positioned mesenteric fat, part of the intussusceptum). The hypoechoic periphery contrasts with the central hyperechoic heterogeneity and contributes to the oft-appreciated pseudo-kidney appearance of a tangential image. This can also be a source of confusion for learners who are well advised to identify the ipsilateral kidney prior to declaring the presence of intussusception. The intussusception is distinguished from adjacent bowel by an absence of peristalsis as well as its non-compressibility.

- Approximately 85-90% of intussusceptions are ileocolic or ileo-ileocolic and are usually located in the right mid-abdomen. Only rarely do ileocolic intussusceptions extend further into the more distal colon. Nonetheless, it is advisable to initiate the sonographic evaluation at the cecum and follow the large intestine to the rectum. Colo-colic intussusception usually presents with rectal prolapse, while ileo-ileal (small intestine) intussusception is usually transient and requires intervention only if associated with signs of bowel obstruction.
- The vast majority of intussusception cases occur in infants and young children. They are thought to be associated with hypertrophied intramural lymph nodes of the terminal ileum intestinal wall. Although these hypertrophied nodes effectively function as “lead points” that are subsequently pushed downstream via normal intestinal peristalsis, this mechanism is considered to be the usual cause of so-called idiopathic intussusception (Figure 5 below). As the nodes are attached to the intestinal wall of the intussusceptum, which is itself attached to extra-mural mesentery containing the vascular supply to the intestine, venous obstruction occurs due to compression between the intussusceptum and intussuscipiens, eventually producing the characteristic “currant-jelly” reddish-purple stool. If not reduced, arterial obstruction will occur as the space between the inner intussusceptum and the containing intussuscipiens continues to entrap and compress its contents with increasing pressure. When intussusception occurs in older children (more than 8 years of age), concern for a causative “pathologic lead point” such as lymphoma or Meckel’s diverticulum is increased.

- Physicians caring for infants suffering from the considerable discomfort of intussusception may, understandably, consider the compassionate provision of potent analgesia discussed in the case presentation. Unfortunately, this well-intended intervention may actually increase infant risk of intestinal perforation associated with the reduction procedure. The administration of narcotic analgesia will often reduce infant resistance to the air enema procedure, specifically decreasing his or her tendency to perform a Valsalva maneuver associated with vigorous crying. The increased compliance effectively decreases extra-luminal intra-abdominal pressure and effects a higher pressure gradient across the intestinal wall, predisposing to bowel distention and perforation due to unopposed intra-luminal positive pressure. Increased extra-luminal pressure exerted by patient resistance conveniently focuses the pneumatic pressure exerted by the air enema against the intussuscipiens in an attempt to return it to its normal position. Other characteristics that predict air-enema-associated-perforation include features indicating bowel wall ischemia, including the absence of blood flow on sonography as well as the prolonged duration of symptoms prior to attempted reduction.
 Figure 6. Intraoperative photograph
Figure 6. Intraoperative photograph



3 Comments
Great articles and great pictures!
Great article , I had this case in my year boards ,,,
Thanks
Just had this Saturday…..u/s image was almost identical. The most prominent symptom my kid had was “lethargy” – didn’t really want to do anything in between bouts of pain.