CT signs of elevated intracranial pressure
Unenhanced or noncontrast brain CT is commonly performed in the Emergency Department to evaluate patients with complicated headache, head trauma, or altered mental status. Emergency Physicians must recognize CT findings of elevated intracranial pressure (ICP) to facilitate appropriate treatment and to avoid contraindicated procedures and therapies. It is important to recognize that CT is an imperfect surrogate for elevated intracranial pressure, which may exist in the absence of radiographic signs. However, when CT findings point to elevation of ICP, the condition should be strongly suspected.
Recognize the CT Signs of Elevated Intracranial Pressure
Evaluation of intracranial pressure using CT requires comparison of cerebrospinal fluid (CSF) spaces. Findings of high intracranial pressure are often symmetrical and may therefore evade recognition, compared with focal lesions such as subdural and epidural hematomas, which draw immediate attention because of asymmetry. In addition to abnormalities of the size of CSF spaces, other abnormalities may be present, including loss of gray-white matter differentiation in cases of cerebral edema.

Examine and Compare the CSF Spaces: a Tale of 3 Spaces and 4 States
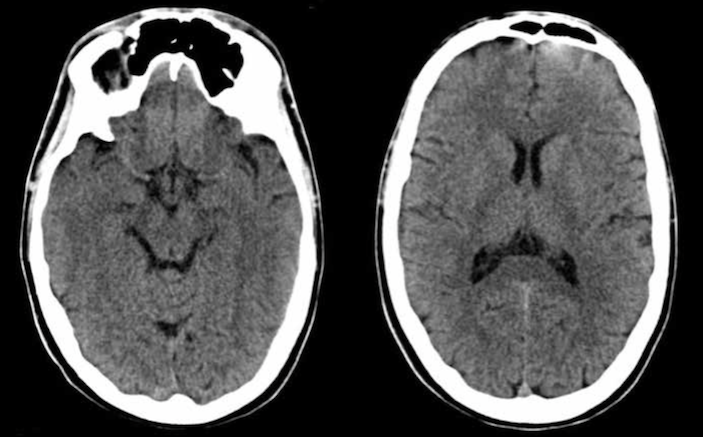
Three CSF spaces should be evaluated: the sulci, ventricles, and cisterns (Figure 1). Patterns of CSF space size and accompanying normal and pathologic states are listed in the table. ICP exists along a continuum, so not all abnormalities may have developed in a given patient at the time of CT. In a normal patient, all three CSF spaces are present, and are neither enlarged nor effaced (Figures 1 and 2). The normal size of the CSF spaces varies with age as described below, and should be considered in the evaluation. In age-related brain atrophy, all three CSF spaces enlarge in response to the loss of brain parenchymal volume (Figures 1 and 3). In cerebral edema, the increased brain parenchymal volume results in effacement of all three CSF spaces (Figures 1 and 4). In obstructive hydrocephalus, the obstructed ventricular system enlarges at the expense of effacement of sulci and cisterns (Figures 1 and 5). Depending on the location of the obstruction of CSF flow, ventricles may be differentially affected. The third ventricle, normally a slit-like midline structure, can become dilated. The temporal horns of the lateral ventricles, normally insubstantial spaces which are barely visible in caudad CT slices, can become dilated and prominent.
Consider the Patient’s Age and Neurologic Status
The patient’s age and neurologic status should be considered when evaluating head CT. Young infants and children commonly lack atrophy, and the paucity of sulci (and small ventricles and cisterns) seen on head CT in these patients may lead to mistaken consideration of high ICP from cerebral edema (Figure 6). However, a normal neurologic exam and level of alertness should cause the Emergency Physician to reconsider that diagnosis, recognizing the CT findings as potentially normal for age. Conversely, patients at advanced age commonly demonstrate atrophy on head CT, so a paucity of sulci should raise particular alarm for elevation of ICP.
Recognize Elevated ICP in the Context of Other Brain Pathology
Elevated ICP can complicate other brain pathology, and may sometimes be overlooked in the presence of another primary brain problem. For example, both meningitis and subarachnoid hemorrhage can precipitate hydrocephalus by creating debris (white blood cells, pathogen debris such as the gelatinous coat of Cryptococcus neoformans, or red blood cells) that prevents reabsorption of cerebrospinal fluid through the arachnoid granulations (Figures 7 and 8). Conversely, when CT findings raise concern for elevated intracranial pressure, a secondary abnormality causing elevated ICP should be considered and sought on CT or through alternative testing – with concurrent treatment of abnormal ICP. Occult underlying causes of high intracranial pressure, not readily recognized on noncontrast head CT, include venous sinus thrombosis and meningitis.
Exercise Caution with Lumbar Puncture
Elevated intracranial pressure is commonly considered a contraindication for lumbar puncture, particularly when mass effect is present. Ironically, several indications for lumbar puncture, including meningitis, subarachnoid hemorrhage, and pseudotumor cerebri (idiopathic intracranial hypertension), are commonly associated with moderate elevations in ICP, even with normal head CT findings. Before performing lumbar puncture, assess carefully for CT findings of elevated ICP as described above.
Reconsider TPA
While elevated intracranial pressure is not explicitly a contraindication for tissue plasminogen activator (TPA or alteplase), CT signs of elevated ICP may point to an alternative cause of neurologic symptoms, rather than ischemic stroke. Consequently, evaluation for abnormal ICP should be a routine part of the diagnostic algorithm for suspected stroke patients, rather than focusing exclusively on exclusion of intracranial hemorrhage.











1 Comment
Great explanation!!