POCUS can be a life-saving tool that can change clinical management when used appropriately.
You have just arrived to the emergency department for the 6 a.m. shift. The census is low and the few patients remaining have all been dispositioned. As you finish taking sign-out, the charge nurse alerts you of a request for a Statement of Refusal (SOR) over the radio.
The paramedic on the other end of the radio informs you of a neonate born just about two hours ago at home who had some persistent difficulty breathing. The local paramedic was notified by the midwife assisting with the delivery who became concerned when the patient did not initially improve with suctioning and supportive care.
As this term newborn female has now improved, the paramedic informs you the parents are refusing transport for further evaluation, noting that “we don’t want any artificial treatment for our newborn.” As you inquire about the patient, the paramedic provides you with a well-appearing, “mottled” sleeping baby with a respiratory rate of 35, rectal temperature of 98.3 Fahrenheit, and 95% on room air. She has attempted to feed once and did not latch very well.
There is mild respiratory distress and some coarse breath sounds. She appears well perfused with normal capillary refill, some mild erythematous on her torso and mildly cyanotic extremities. The rest of her exam is normal per the paramedic. You refuse the SOR and request to evaluate the patient in the emergency department.
On presentation to the ED, the infant appears well, but has some mild respiratory distress with minimal subcostal retractions. She easily cries during the exam and seems a bit fussy. Your exam is similar to the report by the paramedic over the radio, but you also note a full fontanelle.
Furthermore, the patient’s head size is in the 99th percentile on occipital-frontal circumference measurement. After completing your exam and assessment, you order a chest radiograph while monitoring the baby’s respiratory status.
You also consider the patient’s full fontanelle and decide to “take a peek” with the bedside ultrasound machine. You request the microconvex curvilinear transducer because of its small footprint. As the patient is being soothed with some sucrose, you place a small amount of warm gel on the full anterior fontanelle and introduce the transducer in the coronal orientation.
As you tilt from anterior to posterior you note the ventricles appear wider than they should be, which is certainly concerning (Figure 2).

You proceed to acquire additional images of the head US in the sagittal orientation.
Despite your assessment, the patient continues to be stable, appearing sleepy while on room air with mild respiratory distress. You are able to convince the skeptical parents to pursue additional workup. The chest radiograph is read as “no acute cardiopulmonary findings.”
His respiratory status improves after you administer 0.25-liter nasal cannula. She is still fussy but consolable. You decide to a Fast Spin Magnetic Resonance Imaging (MRI) and consult neurosurgery as well. The MRI is consistent with hydrocephalus seen on your bedside ultrasound. The patient is still unable to feed and fails to improve clinically. She is admitted to the neurosurgery service for further management.
Key Teaching Points:
- Transfontanellar POCUS (TF-POCUS) can be used to evaluate the pediatric patient for hydrocephalus, intracerebral hemorrhage, and infectious etiology such as meningitis or an abscess. Much of what we know about this modality among emergency physicians is based on limited case reports, but POCUS can be a life-saving tool that can change clinical management when used appropriately. Although the anterior fontanelle can be open up to two years, the window to acquire reliable images for clinical decision making is between ages 12- to 18-months.[1]
- Hydrocephalus has significant morbidity with late findings that can lead to poor prognosis [1, 2] including delayed neurodevelopment. For infants with shunts, bedside ultrasound of the open fontanelle can serve as rapid, reproducible and a safe way to assess the ventricles. Similar to this case, the indications to perform a TF-POCUS include signs and symptoms of fussiness, poor feeding and vomiting in the setting of a full fontanelle or increased head circumference. This application is a standard for evaluation of the neonate for intraventricular hemorrhage and hydrocephalus and can help guide further examination such as MRI or CT.[3]
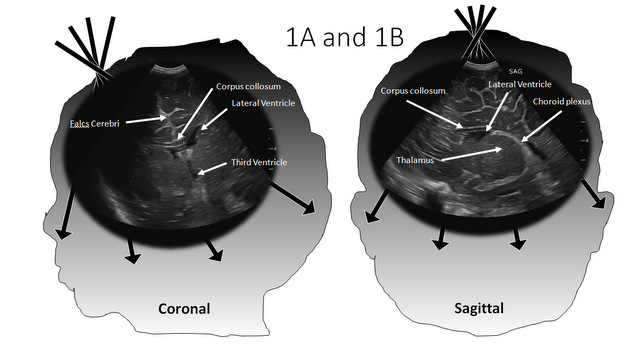
- Understanding the anatomy can augment the emergency physician’s confidence and ability to identify basic anatomy of the ventricles and surrounding structures (Figures 1-3).
 When performing this TF-POCUS exam, there is no specific patient position required, but a calm patient in the caregiver’s lap or supine on the patient’s bed can enhance and optimize the image acquisition and real-time interpretation. Additionally, swaddling the patient, soothing with a pacifier, using warm ultrasound gel and administering timely sucrose drops are good adjuncts to optimize the best results.[1]
When performing this TF-POCUS exam, there is no specific patient position required, but a calm patient in the caregiver’s lap or supine on the patient’s bed can enhance and optimize the image acquisition and real-time interpretation. Additionally, swaddling the patient, soothing with a pacifier, using warm ultrasound gel and administering timely sucrose drops are good adjuncts to optimize the best results.[1] - The transducer of choice for this application is the phased array (preferred) or linear probe, however, the transducer with a smaller footprint able to fit within the boundaries of the neonatal fontanelle is preferred. This includes curvilinear and endocavitary transducers with frequencies ranging between 5 MHz and 10 MHz. Set the desired depth, which is usually approximately 7 cm or enough to visualize the base of the skull.[3]
- Conventional TF-POCUS evaluation is imaged in two planes, a coronal and sagittal plane with the indicator marker pointing toward the patient’s right (for orientation purposes) and toward the anterior aspect of the head respectively (Figure 1). With the transducer in a steady position on the fontanelle, tilt from anterior to posterior for a full coronal view and laterally from one side to the other for a full sagittal view assessment. You should be able to visualize the brain in 3 or more coronal sections (anterior, middle, and posterior views) along with sagittal and parasagittal sections (Figure 1).
- A general anatomical overview of the TF-POCUS will typically show symmetrical small ventricles. Other landmarks to consider include frontal lobes divided by the interhemispheric fissure (on coronal view, Figure 2A), the corpus callosum, and the atrium of the lateral ventricles where the hyperechoic choroid plexus can be visualized. Lastly, if present, blood will appear hyperechoic.[3]
- Sonographic features of hydrocephalus on TF-POCUS include widening (“ballooning”) of the anterior horn of the lateral ventricles with concentric dilation of the frontal horns (Figure 2 and 3).
 Generally, a diameter of the 3rd ventricle more than 1mm in the sagittal plane is concerning for a dilated ventricular system. Alternatively, a temporal horn measurement of more than 3mm is also concerning for dilated ventricle.[1-3] Finally, significant dilation of the ventricles with appearance of thinning of the brain mantle can be seen in severe hydrocephalus as shown in this case (Figure 2).
Generally, a diameter of the 3rd ventricle more than 1mm in the sagittal plane is concerning for a dilated ventricular system. Alternatively, a temporal horn measurement of more than 3mm is also concerning for dilated ventricle.[1-3] Finally, significant dilation of the ventricles with appearance of thinning of the brain mantle can be seen in severe hydrocephalus as shown in this case (Figure 2). 
- As pediatric POCUS utilization at the bedside improves, applications such as TF-POCUS can play a significant role in the clinical exam and initial screening for clinical sequelae such as hydrocephalus, which may present initially with a bulging fontanelle, fussy infant with a known VP shunt, or the neonate with a brief resolved unexplained event (BRUE). TF-POCUS allows the emergency physician to provide a binary answer to whether there is evidence to support hydrocephalus.[3,4]
- While there has been advancement in our understanding of PEM POCUS in other applications, there is a significant void in the use of TF-POCUS in the pediatric emergency medicine department. This includes other indications for this application such as ventricular hemorrhage and intracranial infection, which are yet to be understood. Although evidence to support the use of this application in PEM is limited, there is a potential for TF-POCUS to have a significant impact on how we diagnose hydrocephalus at the bedside for early intervention [1,4].
- It is important to understand that the use of POCUS for TF assessment is an adjunct to medical decision making and should not be used to rule out hydrocephalus at the bedside. In the acute decompensating patient, TF-POCUS at the bedside should not delay computed tomography (CT) evaluation which is the gold standard diagnostic test.
Pearls and Pitfalls
- Avoid a high gain to decrease artifact overexposure.
- The exam is dependent on the anterior fontanelle size and a smaller window may limit the examination. Head positioning may have some effect on ventricular asymmetry which may be misleading, but its area of consequence is uncertain.
- TF-POCUS is operator dependent as with most POCUS applications. Proficiency among the expert POCUS and novice sonographers is yet to be understood.
- Please remember that patient comfort is a key part of image acquisition and assessment in real-time. If available, the use of warm gel, oral sucrose, and placing the infant in the best position of comfort can enhance both patient, caregiver, and sonographer experience.
References:
- Subramaniam S, Chen A, Khwaja A, Rempell R. Identifying Infant Hydrocephalus in the Emergency Department with Transfontaellar POCUS. American Journal of Emerge Med 2019; 37: 127-132
- Yaeger Sk, Marin JR. An infant diagnosed with hydrocephalus by point-of-care ultrasound. Pediatr Emerg Care 2017; 33(4): 287-9
- Pediatric Emergency Critical Care and Ultrasound. 2013. Cambridge University Press
- Thust, S, Nandi D, Hann G. Acting on Macrocephaly in the Neonatal Period: An illustrative case of congenital teratoma. 2014. BMJ Case Rep. cvr2013202742