Why should we care about benchmarks? They are a way to be proactive in evaluating and improving your practice before you get criticized, fired, or have your compensation reduced.

Become a student of your ED’s stats and move from being a reactive to a proactive problem solver
Why should we care about benchmarks? They are a way to be proactive in evaluating and improving your practice before you get criticized, fired, or have your compensation reduced. They can help you move beyond reactive evaluation related to a complaint, a poor patient satisfaction score or a suit, when you might not focus on the best things for improvement. Here are some of the top benchmarks that should matter to emergency physicians.
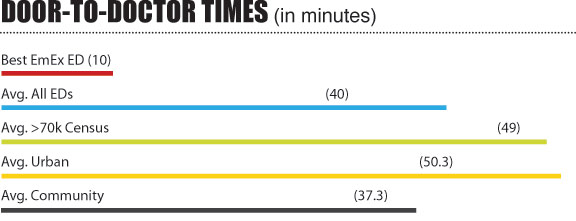
1. Door-to-Doctor Time
The number of minutes from patient arrival to seeing a doctor or a mid level provider is the number one concern for patients and may be the best driver for excellent patient care. We need to find out who is sick in the least amount of time. Meet this expectation and you will satisfy most patients, the administration, and provide high quality care. The “excellent” threshold is less than 30 minutes with the best EDs at about 10 minutes. That said, the average ED has a hard time getting this number under an hour.
2. Door-to-Room Time
The number of minutes that have passed between the patient’s arrival and being placed in a patient care area is the best indicator of your ED’s front end processes. An average performing ED will be about 25 minutes with the best EDs clocking in under 5 minutes. This parameter is largely influenced by the ratio of patients to beds. If you have a lot of patients competing for a few beds, low doctor-to-room times will be hard to achieve. But you can still make it work if you find ways to move the physicians as far forward as possible, using parallel processes instead of serial processing. You can use virtual beds where patients get a brief exam where orders are written and then patients return to a holding area. This allows administration to follow the patient instead of holding up the patient. You must move away from the traditional front-end processing that most EDs are still using. Remember that the patient only remembers how long it took to see the doctor. The fact that he waited an hour in the waiting room and only 5 minutes in the room doesn’t change his impression of the wait. This is a valuable tool in speaking to administrations about changing staffing, facilities, and other bottlenecks that are out of the control of the doctors.
3. Admit Decision-to-Depart Time
Once the decision is made to admit, how long does it take to actually leave the ED? Given the state of EDs around the country, the current “excellent threshold” is 100 minutes. The average of all EDs is a little over 2 hours, but the average ED with a census of over 70 thousand patients is over four hours. In most EDs, in fact, more time is spent on this end of the equation than all of the “value added” time being seen and evaluated by the staff. The question is whether your floors are pulling the patients up or is the ED having to push the patients. This is a question of hospital culture and must be handled with the full cooperation of administration and nursing. And there are lots of ways to improve this number, from streamlining the nurse reporting system to boarding patients in the hallways of the floors to which they are going instead of the ED. This is always a political question that cannot be fixed by the ED leadership alone.
4. Left Without Being Seen (LWBS)
This number is tracked very closely by administration whether EPs like it or not. EPs often view the LWBS patients as those whose illnesses and injuries were not sufficient enough for them to feel they needed to wait, or worse, patients with such a short fuse that we would rather not have them in the ED anyway. Administrators see these patients as lost revenue and increased potential liability. So if you want to stay working at your hospital you must pay attention to this number. The “Excellent Threshold” is 1% or less with the best EDs being much lower. But the truth is that the average ED seeing more than 70 thousand patients has 3% or more of their patients leaving without being seen by a doctor. This number correlates very closely to door-to-room and door-to-doctor times.
5. Satisfaction Survey Percentile Ranking
This falls in the camp of “if it’s important to the administration it must be important to us” despite the flaws in selection bias, small sample sizes and recall bias. To make matters worse, we all know that patient satisfaction is compared on a percentile ranking rather than raw numbers. So if all the physicians or hospitals being compared score very closely, just a few points difference in raw score could push an EP or hospital from the top percentile to the lowest. Nevertheless, these are going to continue to be important to administrators, particularly with the new pay-for-performance initiatives that tie hospital revenues to patient satisfaction.
Realize that some hospital administrators’ pay is tied to patient satisfaction. Further, in the future there will also be more public reporting and hospital-to-hospital comparison of patient satisfaction. So, like it or not, these stats have to be important to us. Ways to improve patient satisfaction are myriad and relate to waiting times, communication, and the perception of care. There are also technical ways to improve scores, however, such as using telephone surveys of larger numbers of patients to dilute the impact of a few vocal unhappy campers.
6. Emergency Physician Perspective of Job Satisfaction
The question is “How professionally satisfied are you with your job?” It’s subjective – and must be anonymous to get a good sample – but it is compared to other subjective surveys. High staff satisfaction is generally reflective of efficiency and staff relationships. The average ED physician is “satisfied”. While it is true that EDs with higher volumes, longer waits and generally lower scores on other benchmarks have the highest reported ED job satisfaction (by a small margin), that is due more to factors such as compensation, flexible scheduling and access to consultants. Higher physician satisfaction is not related to long waits or poor performance.
7. Emergency Nurse Perspective of Job Satisfaction
On average, emergency nurses are less satisfied with their jobs than emergency physicians and this is similarly true with higher volume EDs. This number correlates with nursing staff turnover rates, medical errors, and patient satisfaction.
8. EP Perspective of Nurse/Physician Relationship and Emergency Nurse Perspective of Doctor/Nurse Relationship
These are two related surveys. The “Excellent Threshold” is an average score between good and excellent. If you are getting scores that average less than that, or single scores that score much lower, these must be addressed. Sometimes this is related to staffing levels and/or the division of labor, among other issues. If the leadership is not made aware of these issues until it is too late it will lead to staff turnover, medical errors, and it will hurt patient satisfaction. And we know what that means.
9. PCI Within 90 Minutes
There are clearly better benchmarks of an ED’s clinical competence, but the current public awareness is that this number is related to quality care. We all know of the clinical benchmarks that are either irrelevant or even harmful to quality care. But this just emphasizes that EPs must t
ake charge of what clinical benchmarks are important.
10. Consultant Responsiveness
This is measured by asking the EPs “How responsive is your specialist on-call panel” with the possible responses being 1-not responsive, 4-slightly responsive, 7-mostly responsive, 10-always responsive. The actual numbers on response times are hard to capture due to the decentralized nature of callbacks for most specialists. But it is important to deal with the perceptions. The average ED scores slightly below 7, “mostly responsive”– with the average community hospital scoring the lowest. Though it might not be raw scores, it is helpful to compare one’s own hospital level of responsiveness with others when discussing the issue with administration.
11. Medical Staff Perspective of ED Performance
Whether it’s reality or perception, it is important to know how the medical staff views the ED. The “Excellent Threshold” is 9 out of 10. But the average 70k volume ED is only thought of as “good” by the medical staff. The average community hospital scores only slightly better on this survey. Scoring poorly on this survey can mean that your group is not likely to keep the contract. Scoring well can mean job security and a better place at the table when it comes to negotiating your group’s cut of the bundled payment pie.
Summary: The driving force of benchmarking must be improvement of performance. Benchmarks serve no purpose if they do not reflect the needs and perceptions of all the stakeholders. ED leadership must transition from reactive to proactive problem solving. A dedication to continuous performance improvement through ongoing benchmarked surveys that engage all the stakeholders recognizing and rewarding success will result in a culture of quality.
Mark Reiter, MD, MBA, is the co-founder and CEO of Emergency Excellence, an ED consulting service.



13 Comments
Good day,
I am trying to locate what the national benchmark median is for the above indicators.
Is there such a median?
I would second the above comment — where can we find national benchmarks and medians for the indicators above?
I enjoyed this article; are there references for the benchmarks?
greetings
would you kindly proivde me your refernce for those Benchmarking
Interested in the reference for benchmarks that were stated in the article.
Intially such metrics were from CMS to improve patient care and satisfaction. They have been hijacked by cooperate healthcare to increase profit. A primary metric that results in rushing care and has increased bounce backs is the door to discharge metric or length of stay. In the ER nurses and providers rush under enormous pressure as the ninety minute clock from door to disposition begins to tick. Nurses and Physicians face counseling to job loss when they fail to have satisfactory “numbers.” This is a leading cause of job disatisfaction, burn out, ethical dilemmas and ultimately preventable medical error. Care should always be patient need focused and not satisfactory metric focused. Metrics have little to nothing to do with patient satisfaction and everything to do with cooperate greed.
Hey Mark – I’m surprised I hadn’t seen this article until now. Thanks for doing it.
I’d like to see more debate about the effects of each of these metrics on the individuals delivering care. Sure, we can make dashboards that put these metrics in front of workers so they remain aware of how they’re doing. But isn’t it piling on additional and unnecessary stress? Like Darlene Nelson implies above, it seems like we need a different solution.
I suspect the ideal real-time metric captures the performance of the whole department as interdependent team members, rather than isolating the performance of any particular individual.
I’m not suggesting that the other data should be suppressed. But I think we need to be thoughtful about how individual performance metrics can be expressed to inspire, rather than depress team members.
My question to you…
If you could use ONLY ONE metric on a department performance dashboard, what would it be?
I’d love to discuss this with you sometime. it would be great to cause some lively discussion about these measures, individually.
The benchmarks that I cited are from Emergency Excellence’s database, which includes hundreds of participating EDs. We track 100 different ED performance indicators. You can learn more at http://www.emergencyexcellence.com
This is idiotic. A family of 4 URIs and a septic patient and an MI with CHF who might have a AAA are put into the same “time frame”.
The septic patient and the MI patient aren’t called for patient satisfaction because they’re admitted…… but the family of 4 is.
They are upset because they had to wait, AND the doctor was in a hurry.
Gee, I wonder why?
Hello,
I currently am the Clinical Nursing Director of a Level 1 Trauma Center and Emergency department that is also an Academic Medical teaching center. Is there any data that I can review that measures and compares benchmarks for ED throughput with other academic medical centers? I appreciate your response.
Thank you
Jane
based the performance indicators how you manage staffing ratios to achieve the best for a 400-500 bed hospital
Do we have benchmarks for pediatric EDs?
Pingback: When Integrated EHR Data Isn't Enough | d2i