You are midway through a busy shift when you pick up a chart of a young man with flank pain and vomiting. He was actually seen yesterday in your ED by one of your colleagues who diagnosed renal colic by bedside ultrasound, thus obviating the need for any radiation exposure or even the delays associated with a comprehensive ultrasound by radiology. Unfortunately, now the patient is back with increasing right flank pain despite filling his prescriptions for hydrocodone, ibuprofen and ondansetron. He denies any prior medical history or drug use but did recently travel back home to the Ukraine to visit family.
On physical exam he appears to be in moderated to severe distress, unable to find a comfortable position. His vital signs are normal and other than right CVA tenderness and a few tattoos his physical exam is essentially normal. You note that his urine results sent from triage are already resulted and he does indeed have microscopic hematuria with 50-80 RBC’s per field, 0-5 WBC’s and no bacteria.
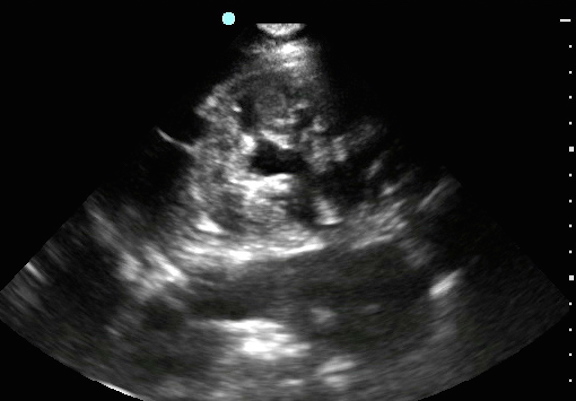
Like your colleague who saw him yesterday you initially decide against a formal imaging study despite this being a “bounce-back” case. You bring in your ED ultrasound machine and obtain the above image. What does it show? After pain management, what should be your next step (Hint: look closely at the entire image)?

Look closely. What do you see? Scroll down for conclusion.

Image one shows definite hydronephrosis in the right kidney (labeled “K”) consistent with ureteral obstruction, most likely from a ureteral stone. The degree of hydronephrosis is probably mild to moderate. This is the dark anechoic area/areas in the center of the kidney (labeled “h”). If you look closely at this image you may also pick up on a second finding. There is some type of cyst or mass on the upper left side of the image (labeled “cyst”). You can only see part of it because it’s tucked up in the corner of the image. It’s easy to miss additional pathology once your search for expected pathology is satisfied by an abnormal finding, in this case the hydronephrosis. This error is sometimes called “search satisfaction.” In other words, the most commonly missed imaging finding is the one you weren’t looking for. This can be even more true when the finding is hiding in the corner of the image. “Corner findings” can be easily overlooked if you are not meticulous, even more so if it is a second and unexpected finding.

A second ultrasound image is shown, now with this hypoechoic mass or cyst closer to the center of the screen. Note there appears to be some hyperechoic calcification between the cyst and the liver that casts a sonographic shadow (labeled “s”). To further delineate this cyst and also to confirm that there was a kidney stone present since this patient was now a “bounce back,” a formal CT urogram was ordered.
Along with that order, to prevent any questions about the care the day prior, the patient was informed “We usually don’t do a CT scan when all we are worried about is a kidney stone.”
The CT showed a 1-2 mm obstruction distal right ureteral stone and a complex cystic mass with calcification and internal echoes that was sandwiched between the liver, kidney and inner thoracic wall. The radiologist raised concern for echinococcus. The patient is sent home with treatment for a ureteral stone and instructions to arrange follow up evaluation for the cyst. Two weeks later the patient’s pain had resolved and he had made an appointment to see a liver specialist, but had not yet had further evaluation.
Pearls & Pitfalls in Performing Renal Ultrasound
- Be Thorough: Image the entire organ by tilting and fanning through the entire region of interest. Don’t just go for one pretty static shot through the middle. By being thorough you are more likely to pick up pathology. If you have a difficult time imaging the left kidney, have the patient hold their breath to bring the kidney more inferiorly. Pay attention to the entire ultrasound screen as you scan. Sometimes important findings may be adjacent to but not actually part of the organ you are focusing on. Any abnormal findings that you are uncertain about should be confirmed with comprehensive imaging, but this can often be done as an outpatient.
- Look for the Hydro: Hydronephrosis is seen as a black or anechoic area in the center of the kidney and represents downstream obstruction.
- Compare Sides: Because most people have two kidneys, any questionable findings on one side may benefit from a comparison view of the other kidney.
- Don’t Forget the Aorta: An aortic aneurysm often mimics renal colic, so always take a look at the aorta, even if your suspicion is low, because it is important to practice looking at normal anatomy. Of course it’s even more essential to pick up an aneurysm before it ruptures.
- Don’t Worry About the Finer Details: During a point of care ultrasound in a patient with known kidney stones, you are not expected to find the stone itself or to look for ureteral jets into the bladder. Concentrate of looking for hydronephrosis.
- Image in Urosepsis: Don’t miss renal obstruction in the setting of urosepsis as relieving the obstruction is a critical part of treatment. These patients may have little to no pain if they are elderly and/or the obstruction has become chronic. Be especially suspicious for obstruction if the patient does not have any other risk factor for UTI.
- Practice, Practice, Practice: The best way to minimize errors is through experience, so scan lots of normal anatomy. The more scans you do, the better you will be able to differentiate abnormal from normal, even when you may not be sure exactly what the abnormality is. An image library of normal and abnormal scans helps immensely, so go to EPMonthly.com and read through some of our previous Soundings columns.
- Stay up to date on how you can use bedside ultrasound to enhance your clinical practice. We’ve created two resources – the ultrasound app “SonoSupport” and Tarascon’s Emergency Department Quick Reference Guide – which you might find helpful.