There are times to consider thrombolytic therapy for PE — and other times when it may just be too risky
A 56-year-old African-American male presented to the ED with palpitations and shortness of breath, which began suddenly at rest just prior to presentation. His symptoms were constant, progressive and worsened with exertion. Associated symptoms included lightheadedness and diaphoresis. He denied chest pain, cough, hemoptysis, fever, or vomiting.
The patient had undergone a left hip resurfacing procedure for severe arthritis eight days before his presentation to the ED, and had complained of increased hip pain and swelling since his discharge four days earlier. He had a remote history of DVT/PE requiring thrombolysis and had remained on Coumadin up until his recent surgery. This medication had been restarted prior to his hospital discharge, but he had failed to continue it as an outpatient. Additional medical history included obesity, hypertension, hyperlipidemia, and sleep apnea. He denied tobacco, drug and alcohol use.
Examination
On examination he was an alert, obese male appearing distressed and acutely ill. His blood pressure was 50/40 mm Hg, heart rate was 170 and pulse-oximetry could not be recorded. He was tachypneic, but his lungs were clear to auscultation bilaterally. His cardiac exam revealed an irregular tachycardia without any murmurs. His abdomen was soft and non-tender. The left lower extremity was edematous and tender in the calf and he was diaphoretic. He was neurologically intact.

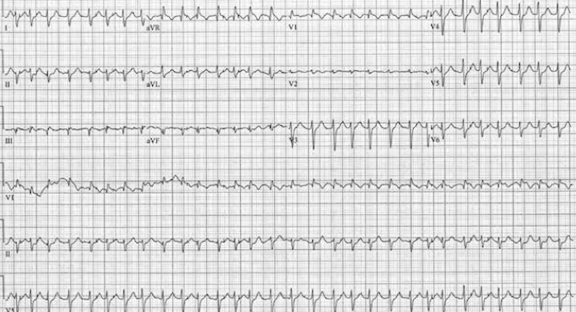
His electrocardiogram showed wide-complex atrial fibrillation with rapid ventricular rate of 182, right axis deviation, right ventricular hypertrophy and inferior Q waves (Figure 1). The initial EKG also showed an S1Q3T3 pattern. Due to hypotension in setting of this arrhythmia, synchronized cardioversion was performed successfully under etomidate sedation with conversion to sinus tachycardia with rate 120 beats/minute (Figure 2). Post cardioversion, his blood pressure improved to 100/70 mm Hg.

His lab results were remarkable for a mild anemia with a hematocrit 35.7%, leukocytosis of 23,000 cells/μL, acute renal insuffiency with a creatinine 1.45 mg/dL, an INR of 1.2 and an elevated troponin to 0.21 ng/mL.
Suspicion of PE
The patient’s presentation was highly suspicious for pulmonary embolism (PE). He was sent to radiology for CT angiography of the chest however he was sent immediately back to the ED due to recurrent hypotension (BP 80/60 mm Hg) and severe orthopnea. He was found to have reverted back to a rapid wide complex rhythm, and he was cardioverted successfully to sinus tachycardia. An amiodarone bolus and infusion was initiated for attempted control of the dysrhythmia.
Due to the patient’s instability, he was intubated using etomidate and succinylcholine. A cordis central venous catheter was placed in the right internal jugular vein using ultrasound guidance. Given the high probability of PE, high-intensity heparin infusion was initiated and cardiology was consulted. A bedside echocardiogram demonstrated a dilated right ventricle and McConnell’s sign —isolated akinesia of the mid-free wall of the right ventricle (Figure 3), findings consistent with right ventricular strain and PE.

Over the course of his ED stay the patient repeatedly developed a wide-complex tachycardia resembling ventricular tachycardia or atrial fibrillation with rates as high as 240 beats/minute with associated marked hypotension with systolic pressures as low as 50 mm Hg. The dysrhythmia recurred eight times and each of these episodes responded to cardioversion, with improved hemodynamics.
Risk of Bleeding
Thrombolytic therapy was considered; however it was thought that due to the patient’s recent surgery this treatment would incur an unacceptable risk of bleeding. Cardiothoracic surgery was consulted and elected to take the patient to the operating room for an embolectomy. By this time the patient had retained hemodynamic stability and was able to undergo CT angiography of the chest that confirmed diagnosis of a saddle PE (Figure 4).

The patient was then admitted to the OR where he underwent an embolectomy (Figure 5) by way of a median sternotomy, along with closure of a patent foramen ovale. In addition, a single vessel coronary artery bypass grafting with reverse saphenous vein graft to the right coronary artery due to persistent intraoperative right ventricular dysfunction was performed.
His hospital course was remarkable for development of persistent atrial fibrillation. He had an IVC filter placed and warfarin therapy was resumed. He was discharged on post-operative day 11 to cardiac rehab and then home on day 18 in good condition.
Discussion
Pulmonary embolism (PE) is a major health problem, affecting approximately 1 in 1000 people in the US and ranking as the 3rd most common cause of death in hospitalized patients [1]. More than 80% of PEs are associated with DVT in hospitalized patients [2]. Major risk factors for development of PE include immobility, recent trauma or surgery (especially hip or spine procedures), and obesity [2].
While PE may be asymptomatic in up to half of afflicted patients, large thromboemboli may cause significant cardiovascular compromise [1]. The most common ECG finding in PE is sinus tachycardia; however right ventricular strain may manifest as precordial T-wave inversions, right bundle-branch block and the S1-Q3-T3 pattern. Severe right heart strain may also lead to hypotension and acute heart failure, and is the culprit for 5-25% of cardiac arrest victims. PEA is by far the most common rhythm seen in these cases, followed by asystole and ventricular fibrillation [3]. PEA is thought to predominate due to obstructed pulmonary blood flow in the heart with a healthy electrical conducting system; however a heart prone to arrhythmia may manifest alternative rhythms [4].
Treatment of the PE leading to cardiac arrest is largely an academic discussion. ACLS and CPR are standards of care and EM dogma recommends tPA in cases of proven massive PE or tPA consideration in cases of suspected massive PE [5]. The American College of Chest Surgeons also recommends thrombolytic therapy for confirmed massive PE [6]. However, large clinical trials are lacking and results of large PE registry data have shown mixed results with respect to patient mortality [7]. Furthermore, in many cases tPA is contraindicated, such as in the case presented; thus alternative treatment methods such as embolectomy must be sought.
Embolectomy is an option for those with cardiogenic shock, for those who fail medical or thrombolytic therapy, or for those in whom thrombolytic therapy is contraindicated. In case series, outcomes for these patients are generally favorable with respect to the critical illness, especially in cases of early intervention [8,9]. In spite of these studies, there are no widely accepted guidelines for surgical management of massive pulmonary embolism [10].
REFERENCES
1. Ouellette, Daniel, et al. Pulmonary Embolism. Medscape, 2013. www.emedicine.mescape.com
2. Kline, Jeffrey A. “Thromboembolism.” Tintinalli’s Emergency Medicine. Ed. Judith E. Tintinalli. New York: McGraw Hill Medical, 2011. 431-41. Print.
3. PE as cause of cardiac arrest, Arch Intern Med, 2000 May 22:160(10):1529-35) (The incidence of PE in unexplained sudden cardiac arrest with PEA, Am J Med. 2000 Oct 1;109(5):351-6.
4. Acute Myocardial Infarction and Massive Pulmonary Embolus Presenting as Cardiac Arrest: Initial Rhythm as a Diagnostic Clue, Case Rep Emerg Med. 2013; 2013: 343918.
5. Advanced Cardiovascular Life Support Algorithm, American Heart Association, 2014.
6. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition), Kearon et al, Chest. 2008 Jun;133(6 Suppl):454S-545S.
7. Massive Pulmonary Embolism, Kucher et al, Circulation. 2006 Jan 31;113(4):577-82. Epub 2006 Jan 23.
8. Early and late clinical outcomes of pulmonary embolectomy for acute massive pulmonary embolism, Vohra et al, Ann Thorac Surg. 2010 Dec;90(6):1747-52.
9. Aggressive surgical treatment of acute pulmonary embolism with circulatory collapse, Takahashi et al, Ann Thorac Surg. 2012 Sep;94(3):785-91.
10. Pulmonary embolectomy: recommendation for early surgical intervention, Carvalho et al, J Card Surg. 2010 May;25(3):261-6.



1 Comment
What would you have done in rural hospital 3-6 hrs (depending on weather) from cardiothoracic surgery? Is the risk of hemorrhage after hip resurfacing so great that tPA would be contraindicated?