Your patient has had a series of elective abortions, but her recent D&C has left her in considerable pain and wondering why she’s missed two periods.
One of your first patients on the night shift is a mother of three presenting with two days of gradually worsening pelvic and low back pain. She denies any fever, vomiting, diarrhea, dysuria or vaginal discharge or bleeding. She does mention that about two months ago she had a dilation and curettage (D & C) for an unwanted pregnancy and has not had her period since. She states she has actually had a total of four prior elective abortions and this is the first time where she had very little bleeding afterwards. She also feels that it is odd that she has skipped two periods because she is usually quite regular. She is sexually active with her husband but she did a home pregnancy test yesterday and it was negative.
On exam her vitals are normal and her general exam is unremarkable except for suprapubic tenderness with guarding but without rebound. On pelvic exam there is cervical motion tenderness but no discharge or other abnormal findings. A CBC, UA and pregnancy test sent from triage as a protocol are also normal.
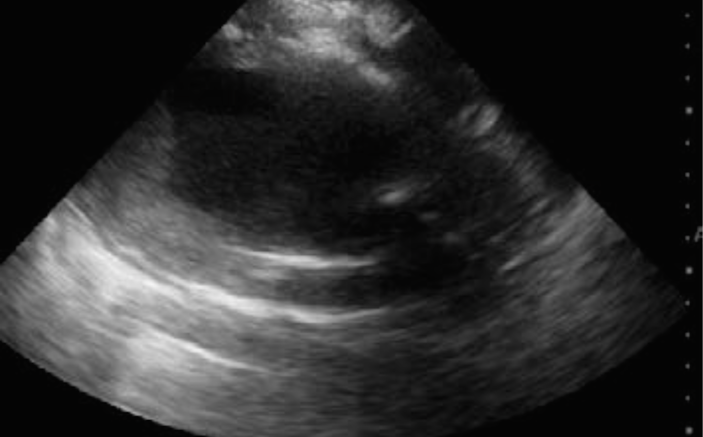
You decide to take a look with the ED ultrasound machine. Unfortunately, your patient recently urinated in order to provide a sample in triage, so you don’t have the best acoustic window. Nevertheless, you are able to obtain some decent images of the uterus. Here are two of them. Test yourself. Slide the bar to see what they show?
[twentytwenty]



The uterus is enlarged and filled with gray echoic clot and black anechoic blood. Image 2 also shows some posterior enhancement, a common hyperechoic artifact deep to a fluid filled structure. Although it is not measured with calipers, by using the centimeter markers on the right side of the screen you can estimate the thickness to be about 8-9 cm thick. The 16 at the bottom right corner of the screen marks a depth of 16 cm from the probe. Each dot is 1 cm and the thicker dots are each 5 cm from each other. The normal uterine thickness is about 3 cm (The normal uterine dimensions in a woman of reproductive age is about 7.5 cm long, 4.5 cm wide and 3.0 cm thick).
The patient was presumed to have some obstruction to menstruation, but obviously not an imperforate hymen. The gynecology service was consulted and the patient was diagnosed with uterine cervical stenosis, presumably due to multiple prior abortions. The gynecology resident attempted to pass a probe into the uterus to dilate it but the patient was unable to tolerate the procedure. Her attending physician asked for her to be sent to his office where he performed a nerve block and was able to dilate the cervix and release the backed up blood.
Discussion
Uterine cervical stenosis is a rare condition that results from obstruction to menstrual outflow and therefore an accumulation of blood in the uterus (hematometra). Symptoms may include pain that is typically most severe at the time of expected menses, amenorrhea, urinary frequency from pressure on the bladder, and infertility. Imaging showing a uterus distended with blood and/or clot supports the diagnosis, but the definitive diagnosis is made by inability or excessive difficulty trying to pass a probe through the cervical os into the uterus. Complications may include infection or the backflow of blood products through the fallopian tubes into the pelvis. Treatment is with cervical dilation via metal dilators and/or a cervical stent or luminaria.
Pearls & Pitfalls in Transabdominal Pelvic Ultrasound in the Non-Pregnant Patient with Pelvic Pain
- Basics: Although transvaginal ultrasound is more sensitive than transabdominal ultrasound for the evaluation of the female reproductive organs, the ED physician rarely needs to perform a trans-vaginal scan. With a trans-abdominal you can usually tell if there is any pathology that requires emergent treatment, such as a huge cyst at risk for ovarian torsion, a big abscess, or other major condition. When there is concern for a less emergent condition such as a routine ovarian cyst, a formal ultrasound should be ordered.
- Free Fluid: Fluid tends to accumulate between the bladder, which will always be anterior, and the uterus. Very small amounts of free fluid soon after ovulation may be physiologic, but would rarely be noted on a trans-abdominal ultrasound. Larger amounts of fluid may have the appearance of cat ears, or if a bit larger may look like a bow-tie. Rarely hemorrhagic cysts in non-pregnant patients can cause massive internal bleeding. If there is a large amount of free fluid, emergency surgery could be indicated, especially if it tracks into Morrison’s pouch, even if the pregnancy test is negative. For some examples of the appearance of free fluid on ultrasound visit the “EM Ultrasound” webpage at EMresource.org and choose “Obstetrics/Gyn” on the right..
- The Uterus: The normal uterine dimensions in a woman of reproductive age is about 7.5 cm long, 4.5 cm wide and 3.0 cm thick. These measurements are typically smaller during premenarche or menopause.
- The Endometrium: The normal endometrial stripe thickness varies but, is usually <15 mm during the reproductive years and <5 mm during menopause. Thickness can change depending on the phase of the menstrual cycle, during menopause, or with the use hormonal therapy or Tamoxifen. After an abortion the thickness should be <5 mm.
- The Ovaries: Normal ovaries in a woman of childbearing are usually 3-5 cm in length. Simple cysts under 2.5 cm in diameter are often painless but complex or hemorrhagic ovarian cysts that are smaller or simple. Cysts that are larger than 2.5 cm often cause pain. Pain from an ovarian cyst usually starts mid-cycle and usually ends by menses. Cysts between 5-10 cm are highest risk for ovarian torsion. Cysts smaller than 5 cm and those larger than 10 cm are less likely to torse. In infection, tubo-ovarian abscesses (TOA) may occur. If you want to see an image of an ovarian torsion and a TOA go to the “EM Ultrasound” webpage at EMresource.org and choose “Obstetrics/Gyn” on the right.
- Practice, Practice, Practice: Whenever you scan for alternate indications in women, practice looking at the pelvis with trans-abdominal ultrasound. The more normal patients you look at, the more likely you are to recognize when something is not right. With bedside ultrasound there is no substitute for experience. The more ultrasounds you do, the better you will be able to differentiate abnormal from normal, even when you may not be sure exactly what the abnormality is. An image library of normal and abnormal scans helps immensely, so check out our Soundings library.
- Over-zealous administration of the local anesthetic within the nerve is not necessary and may cause nerve damage. Deposition of local anesthetic adjacent to the epineurium is adequate for satisfactory anesthesia.



9 Comments
I have a lower back pain after 12 days of abortion. This is my second abortion in seven months. Is there any problem..?
I had a number of abortions before giving birth 10 years ago. I’ve had a couple of them afterwards and I have a very severe lower back pain for the past 4 years. Could the abortions be the reason for what I’m going through?
Hi I’m NAD but I had an ovarian cyst along w a pool of blood in my uterus like this woman as well as tissue still in there from a failed medical abortion. My back pain was more severe in the side I had the cyst and the pain wrapped around to that side of my pelvis. I thought it was just from my hip problems and that the hip was stuck until it popped once and I found no relief. I also had pain so bad that I had to stop walking inside stores randomly. Driving also became painful/uncomfortable.
Please am having pelvic nd back pain since i did an evacuation last year and it ve been so painful i cnt even bend down nd since that last year i ve been going to hospital taking some drugs but to no avail please what else can i do nd how can i treat myself or what medications can i take to get relieve because am now worried, thank you.
I’m having serious back pain after miscarriage any solution
Its been two months since I had An evacuation but I sometime have excruciating pain on my abdomen, what could be the causing the pain?
I had abortion about 3 weeks,and ever since then I have been battling with back pain over 3 month now,pls what can I use,I’m tired now ,the pain is serious please
Take some muscle relaxants like paracetamol tablets ,then u Will fill better
I had my abortion one week ago, and im still habing a lower back pain that come amd go… When i take ibuprofen, pain will stop… But after few hours it come again… Not severe pain but enougj for me not to feel comfortable… Anybody could help me here pls.