Can bedside ultrasound provide an alternative to your standard – painful – abscess care?
You look up at the clock and can’t believe how fast the night has gone by already. It’s already 4 am and nearly every bed in your ED is filled with hospital admissions. The flu season has been incredibly taxing on your community and your hospital, and it doesn’t seem to be letting up any time soon. Exhausted and hungry, you would like nothing more than to take a quick break, but you look at the tracking board and there are still patients waiting to be seen. You walk out to the waiting room to see who else may need your help tonight.
Amidst the empty chairs recently vacated by those who grew tired of the wait, you see a young girl sitting all by herself, wrapped in a blanket, sound asleep with her head against the wall. Not wanting to disturb her right away, you ask your triage nurse what the story is.
“She’s been here for hours, doc.” Your triage nurse says with a yawn. “She checked in with an arm infection, but got bumped by all of the ambulance traffic. Do you want me to walk her back now?”
“No worries. I’ll take her back with me.” You reply, as you gently nudge the young girl awake.
“Hi, I’m sorry to startle you. We’re ready to take you back and see you now.” Your kindness is met with a gentle smile and nod of her head.
In one of you last empty rooms in the ED, you sit down next to the young girl and start your assessment. She is 18 years-old and she is concerned about some redness that has developed over her forearm. It started off as a small ingrown hair that she tried to pluck out with tweezers. Over the last couple of weeks, it has become more swollen and angry looking so she finally decided to come into the ED.
She is wearing a long sleeved shirt to cover up her arms despite it being quite warm outside. You ask her why she didn’t see a doctor earlier, and she replies bashfully that she didn’t know what to do. Her parents recently passed away in a car accident and she has been living by herself, trying to navigate the world alone.
Your heart goes out to her as you see her rub away tears in her eyes. “Please don’t cut me open, doc.” she cries. You console her and reassure her that you will take good care of her as you turn your attention to her forearm and notice some swelling with overlying erythema. The quick and simple plan would be to provide some local anesthesia, make an incision with a scalpel, insert your curved Kelly clamps to explore and break up any loculations that may have formed, pack her abscess, and have her follow up. You’ve done it hundreds of times, but tonight, you decide that you are going to try something new.
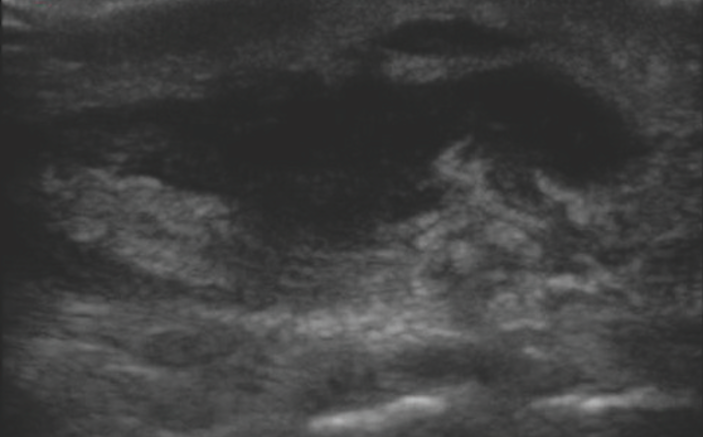
With the high frequency linear array transducer, you perform a bedside, point- of-care soft tissue ultrasound evaluation of her forearm. You obtain the following images (Image 1 and Image 2 below).
Based on these images, what other treatment approaches can you try?


On your bedside ultrasound, you note a simple hypoechoic abscess pocket that appears quite superficial. Using the depth markers on the side of the ultrasound image, you note that the heart of the abscess pocket is only about a centimeter from the surface. There are no septations or loculations, and the pocket still appears dark black and liquefied.
You take a moment to gather some supplies to help you with the task at hand: a 3 mL syringe, a small gauge needle, lidocaine with epi, an 11-blade scalpel, and a small flexible suction catheter. After injecting a small amount of local anesthetic over the abscess, you make a small stab incision just wide enough to slide your catheter tip through. You insert your catheter tip and gently suction out all of the pus in the abscess pocket. A repeat ultrasound of the pocket shows you that you have suctioned out all of the pus, and you didn’t have to apply any pressure or cause any further inflammation or pain by trying to squeeze and push the pus out of the abscess with your fingers. By limiting the size of your incision, you hope that it doesn’t leave as much of a scar on this beautiful young girl’s arm.
To minimize chances of the abscess re-accumulating, you decide to tie a vessel loop through the incision you made and you teach the patient how to cut and remove the vessel loop in 5-7 days. She is so thankful for your compassionate and thoughtful care that she almost knocks you over with her hug of gratitude.
Walking out of her room, you see that your nursing team has left you a small token of appreciation. At your desk you see a scalpel taped to a cookie and a note that reads, “Thank you for always remembering why we do what we do…All it takes is a small act of kindness and compassion to keep our profession a cut above the rest.”
Tips & Tricks For Ultrasound Guided Abscess Drainage
- Ultrasound can be used at the bedside to help guide your approach to drainage of an abscess.
- Use a high frequency linear array transducer and begin by scanning the normal surrounding soft tissue. Slide your probe towards the inflamed area of interest and note any nerves or vessels that may be adjacent to or overlying the abscess.
- Abscess pockets will appear dark black and anechoic or hypoechoic during the initial stages of formation. As the inflammatory process progresses, the pus may begin to appear more heterogeneous with a mix of hypoechoic and hyperechoic material swirled together.
- Scan through the abscess pocket and look for bright white, hyperechoic septations and adjacent hypoechoic loculations.
- If the abscess pocket appears as one simple pocket of fluid without any septations or loculations, consider minimizing the amount of local tissue damage and inflammation by making a small incision and inserting a suction catheter into the middle of the abscess. This technique works best with abscesses that are still mostly liquefied and appear dark black and anechoic on ultrasound. A larger suction catheter may be required for thicker, more hyperechoic pus noted on ultrasound.
- Ensure that you have suctioned out as much purulent material as possible by re-evaluating the abscess pocket with ultrasound.
- If you think that the abscess pocket may re-accumulate and you want to avoid using traditional packing techniques, consider using a vessel loop, thin penrose drain, or cutting a thin strip of a sterile glove, tourniquet, or the tubing from a butterfly needle for your “incision and loop drainage” of the abscess. More information about this technique can be found with a simple internet search for “incision and loop drainage of abscesses”.
- If you instruct your patient to return for a follow-up evaluation for their loop removal, evaluate the site first with point-of-care ultrasound to ensure the pocket is healing without complications before removing the loop.
- Stay up to date on how you can use bedside ultrasound to enhance your clinical practice and improve patient care. Check out the ultrasound app “SonoSupport” available now for smartphones and tablets.



1 Comment
It would be really nice if you could post a video or videos showing the ultrasound being performed. Thank you for considering.