 You just sent someone home with peripheral vertigo . . . or was that a stroke? Before we break down an approach to vertigo, let’s briefly consider two questions: just how often does this “nightmare” scenario occur and does it really matter anyway?
You just sent someone home with peripheral vertigo . . . or was that a stroke? Before we break down an approach to vertigo, let’s briefly consider two questions: just how often does this “nightmare” scenario occur and does it really matter anyway?
You just sent someone home with peripheral vertigo . . . or was that a stroke?
Before we break down an approach to vertigo, let’s briefly consider two questions: just how often does this “nightmare” scenario occur and does it really matter anyway? Despite some earlier studies highlighting the frequency with which clinicians misclassify central causes of vertigo as peripheral, some very reassuring data was recently published by a group in San Francisco. In their study recently published in the Annals of Emergency Medicine, Kim et al. tracked all patients discharged from California emergency departments with a primary diagnosis of dizziness or vertigo in the first half of 2005. In their sample of 31,159 patients, less than 1 in 500 returned to hospital with a stroke in the first month after discharge. When one considers that at least 2% of all cases of myocardial infarction and acute coronary syndrome are missed in the ED, this number of missed transient ischemic attacks or strokes doesn’t seem too bad.
Nonetheless, there was a very prominent clustering of cases of death or hospitalization from cerebrovascular causes in the first two months after discharge. In other words, there is room for improvement – a significant number of patients with transient ischemic attack and stroke are indeed being missed.
To answer the second question (whether it matters), we have to consider whether we have any effective therapy for these patients beyond oral antiplatelet agents like aspirin. We do – at least for many of them. Although patients with ischemic symptoms in the posterior circulation are not candidates for carotid endartectomy or stenting, a greater number proportionately will be found to have atrial fibrillation or other sources of emboli. In patients with TIA or minor strokes of the posterior circulation, anticoagulation may present an opportunity to forestall disaster.
The key to the evaluation of the patient with vertigo is to first determine if it is isolated. The cerebellum and brainstem, both supplied by branches of the basilar artery, are proportionately much smaller than the cerebral hemispheres. Thus, it is very difficult for ischemic lesions to affect only the central vestibulo-cochlear (8th) nerve nucleus without affecting other cranial nerves. So, if vertigo is not accompanied by other symptoms or signs pointing to the brainstem or cerebellum, it is relatively unlikely that it is of central origin, and even less likely that it is due to a posterior circulation stroke. To remind us of the signs that we are looking for, the nmemonic of the five D’s is helpful: dizziness (vertigo), diploplia, dysarthria, dysphagia and dysmetria (cerebellar ataxia). In addition, the presence of any long tract signs, that is, any motor or sensory changes in the extremities, also should lead the EP to assume a central cause of vertigo. The one exception to this rule is when vertigo is accompanied by tinnitus or partial hearing loss. Because these symptoms are most commonly a result of pathology in the sensory organs themselves, their presence points to a peripheral source. Meniere’s disease, characterized by acute attacks of severe vertigo associated with tinnitus and hearing loss is the classic example. Although a complete neurological examination is necessary in patients with vertigo, perhaps its most critical component is gait testing. Although patients with peripheral causes of vertigo may have some difficulty with balance, they are generally able to walk. Inability to walk remains a key red flag that should prompt consideration of further evaluation and admission.
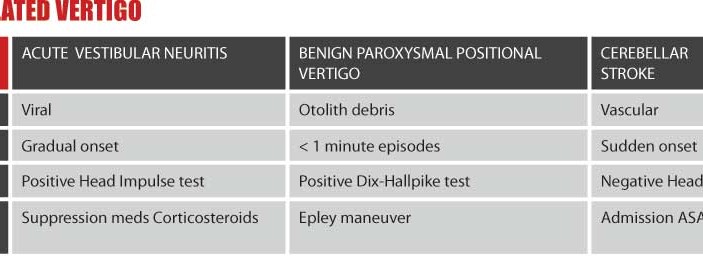
Unfortunately, even if vertigo is truly isolated, there is still a small chance that one might be dealing with a cerebellar stroke. To distinguish cerebellar stroke from the two other major causes of isolated vertigo (which are both peripheral), the accompanying table is helpful. The key differences are in the temporal pattern of symptoms. Unlike the extremely brief (seconds long) episodes of benign paroxysmal positional vertigo and the insidious onset of vestibular neuritis, cerebellar strokes typically are sudden in their onset, but of longer duration than benign paroxysmal positional vertigo.
click on image to enlarge
Of the two diagnostic maneuvers listed on the table, more EPs are familiar with the Dix-Hallpike. We should be careful when interpreting this test. It should only be considered positive when a patient without vertigo at rest has vertigo and torsional nystagmus beginning briefly after the sudden change in position and then resolving less than a minute. The head impulse test is even easier to perform than the Dix-Hallpike but has only recently gained recognition in the emergency medicine community. To perform the head impulse test, one simply asks the patient to maintain their gaze on the examiner as the head is quickly rotated to each side. The presence of corrective saccades when turning to the given side is suggestive of a peripheral source on that same side. A negative head impulse test thus may raise one’s suspicion of a cerebellar stroke. (Learn more about both tests on Mel Herbert’s online video.)
So, perhaps this will take a bit of the groan out of your next encounter with a patient with vertigo. After you make sure that it’s isolated, remember the ABCs: acute vestibular neuritis, benign paroxysmal positional vertigo and cerebellar stroke.
Dr. Swadron is Vice-Chair for Education and Residency Program Director in the Dept of EM at LA County/USC Medical Center. He is an Assoc. Prof. of Clinical EM at USC’s Keck School of Medicine of the University. EM:RAP (Emergency Medicine: Reviews and Perspectives) is a monthly audio program that can be found at www.EMRAP.org




6 Comments
I have had much more conflict with computer issues, especially now that our hospital refuses to pay for our dictations and we have switched to Powernotes and Dragon. Very distracting, disturbing and has seriously affected my ability to practice emergency medicine.
I worked in a rural hospital in which the administrator came to the
ed and triaged patients according to their ability to pay. Also, it was routine for consultants to refuse care to the poorly insured. They neither understood nor cared to understand emtala law.
I didn’t get over it. I resigned. If I knew how, I would report them.
Most conflicts that I have seem to come from false expectations of what I can or should provide to patients in the emergency room (E.G. “I have this rash for one year, can you tell me what it is?”, or “I want an MRI because my doctor has not ordered me one and I have this pain for 3 months already”, or “what do you mean you can’t tell me if I have a heart problem unless I am admitted for a stress test?”)
I would assume that you perform the head impulse test prior to the Dix-Hallpike test?
couldn’t find the “video” of head impulse test, where is it?
I couldn’t find Mel’s video on the head impulse test but here is another site http://www.medscape.com/viewarticle/710698