While risk factors for Clostridium Difficile Associated Disease (CDAD) are well known, how often are they asked of patients in the ED? While the standard diarrhea questions regarding camping; drinking of stream water; sick contacts; and travel are rarely overlooked, antibiotic exposure and hospitalization—the chief risk factor for CDAD—must be ascertained. Many emergency physicians would likely be surprised to discover that C. difficile can be a community pathogen (a la ca-MRSA) and can occur in patients without standard risk factors

One study addressing these issues is a Canadian study published in 2003. This study reviewed ED admissions for CDAD and found that 44% of cases were community acquired, i.e. in patients who did not reside in a nursing home or have a history of 24 hours of hospitalization in the past 60 days. Not surprisingly, the majority of the case patients had received antibiotics [1].
With the advent of the hypervirulent ribotype 027 (BI/NAPI) strain of C.difficile it is not surprising that, with its heightened pathogenicity, it is capable of causing disease in hosts not typically thought susceptible. In 2005, the MMWR published case reports of two such cases occurring in Pennsylvania. One was a fatal case in a pregnant woman who spontaneously aborted a twin pregnancy and whose only antibiotic exposure was TMP/SMX 3 months earlier and the other occurred in a 10 year old girl without antibiotic exposure. These two cases prompted further investigation which uncovered 23 community acquired cases and 10 peripartum cases. Ominously, 24% of the cases reported no antimicrobial exposure [2].
In January 2006, Connecticut added community-acquired CDAD to the list of reportable conditions and after a year of reporting discovered an incidence of 6.9 cases per 100,000 population (241 cases).
–Females represented twice as many cases as men
–Rates higher in spring and summer
–46% required hospitalization (median length of stay: 4 days)
–12% required ICU admission
–2% died
–29% had an inpatient health-care exposure >3 to 12 months preceding illness
–67% had an underlying medical condition
–68% had taken an antimicrobial during the 3 months preceding symptom
–25% patients had no underlying conditions and no inpatient health-care exposures during the 12 months preceding illness. This group was younger, less likely to require hospitalization, and more likely to report bloody diarrhea
–Coinfection with a second pathogen appeared to be rare.
–2% had a stool-culture positive result for another reportable enteric pathogen [3]
Emergency physicians should consider CDAD in their patients, first and foremost, in those with traditional risk factors. However, in light of the appearance of C.difficile in the community, it should be added to the differential diagnosis in several other patient groups:
–Anyone with diarrhea after antibiotic exposure should be considered a possible CDAD case
–Anyone with diarrhea after health-care contact (e.g. hospitalization, nursing home residence, dialysis center attendance)
–Certain unexplained diarrhea cases that are bloody or associated with leukocytosis and/or fever
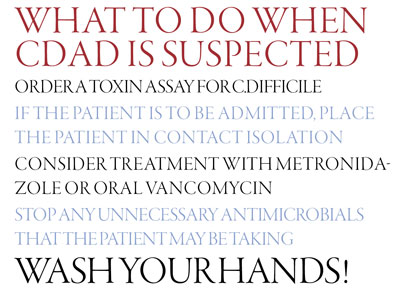
1. Order a toxin assay for C.difficile
2. If the patient is to be admitted, place the patient in contact isolation
3. Consider treatment with metronidazole or oral vancomycin
4. Stop any unnecessary antimicrobials that the patient may be taking
5. Wash your hands!
1. Andrews CN, Raboud J, Kassen BO, et al. Clostridium difficile-associated diarrhea: Predictors of severity in patients presenting to the emergency department. Can J Gastro 2003;17:369-73.
2. CDC. Severe Clostridium difficile–associated disease in populations previously at low risk—four states, 2005. MMWR 2005;54:1201–5.
Dr. Adalja, board certified in both emergency medicine and internal medicine, completed a fellowship in infectious diseases and is currently a fellow in the Department of Critical Care Medicine at the University of Pittsburgh Medical Center.