A helpful application of the Canadian C-Spine Decision Rule, or an onerous malpractice risk?
A helpful application of the Canadian C-Spine Decision Rule, or an onerous malpractice risk?
Looking around your ED on another cold winter night, you vividly imagine catching up on the 40+ patients yet to be evaluated in the waiting room sometime over the next 12-hours. When your charge nurse informs you that the weather forecast projects “black ice” tonight, you grimace. Two hours later when the tenth motor vehicle accident victim from the ice-rain arrives via EMS boarded and collared, you are ready to scream since your waiting room now has over 60 patients. As you survey your resources, you wonder whether the triage nurses might help alleviate the MVA patient’s discomfort by applying validated criteria to quickly evaluate their blunt neck injuries and identify which patients might await further evaluation without a cervical collar.
Options
1. Keep all of the patients in cervical collars and let them wait their turn in the triage cue.
2. Quickly educate your triage nurses about one of two validated cervical spine injury clinical decision aids (NEXUS or Canadian) and put them to work evaluating the onslaught of MVA patients.
3. Efficiently extricate yourself from the busy ED to personally evaluate all of the MVA patients in triage in order to make physician-based decisions about cervical spine clearance.
The Critical Question:
Can trained triage nurses accurately and comfortably apply the Canadian C-spine rule to adult blunt trauma patients who are alert, cooperative, and hemodynamically stable?
The Bottom Line
Triage nurses in university and small community hospitals can be trained to accurately identify a subset of blunt neck injury patients as low-risk for clinically significant cervical spine injury. Most triage nurses are comfortable applying the Canadian c-spine rule to these patients. The majority of “misses” occur early in the training process and involve failure to recognize a “dangerous mechanism”.
About one-million patients present to U.S. emergency departments each year following blunt neck trauma and over 97% will be found to have no cervical spine instability or fracture. The majority of these patients are alert and otherwise stable, but most EMS protocols nonetheless mandate cervical spine immobilization since the consequences of a missed injury can be catastrophic. Unfortunately, “boarded and collared” patients can wait in discomfort for hours until clinical or radiographic clearance from spine injury. In addition to patient discomfort current practice can aggravate ED overcrowding.
The occurrence of cervical spine injury is negligible in rear-end collisions, as opposed to high risk mechanisms such as axial loads, falls, and diving accidents. Clinician fear of missing an injury has resulted in significant variation in radiographic imaging practice patterns. Consequently, two clinical decision aids have been developed and validated over the last decade: NEXUS and the Canadian C-spine rule (CCSR).
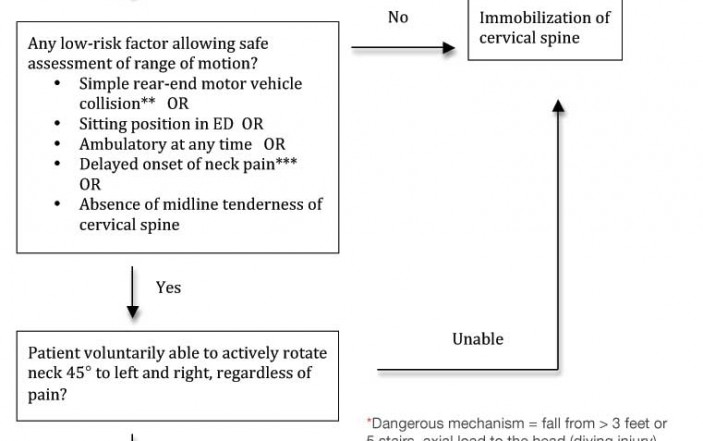
Head-to-head trials have demonstrated the superiority of the CCSR over the NEXUS criteria (sensitivity 99.4% versus 90.7% for CCSR and NEXUS respectively; specificity 45.1% and 36.8%, respectively). In addition, previous trials have shown that the CCSR (Figure) can be accurately applied by pre-hospital and nursing personnel. Amongst physicians the CCSR outperforms unaided clinical gestalt and would safely reduce current imaging practices, if employed.
The current research is a prospective trial in six hospitals (two large teaching, four small community) in the Ottawa Ontario region from 2005 until early 2008. Investigators enrolled consecutive adult patients in stable condition with potential cervical spine injury after blunt trauma. To be included, patients had to be alert and cooperative with a GCS 15 with normal vital signs as defined by the Revised Trauma Score. They also had to present within 48-hours of injury. Patients were excluded if they were under age 16, had penetrating trauma, or had known vertebral disease. Prior to the onset of the trial, triage nurses had a computer-based one-hour training session followed by a one-hour practical session led by a nurse educator reviewing case studies and demonstrating techniques. After the nurse educator graded each participating triage nurse with a performance check list, each nurse had to complete and pass a written test to be certified for cervical spine assessment. The investigators also conducted brief retraining sessions over the course of the study and maintained newsletters to participating nurses. Patient neck immobilization was not actually removed in this validation trial. Instead, nurses simply recorded their interpretation of the CCSR and the patients were maintained in their cervical collars.
The gold standard against which triage nurse CCSR interpretations were compared was investigator interpretations of the primary outcome based on review of all clinical notes. The primary outcome was clinically important cervical spine injury defined as any fracture, dislocation, or ligament instability requiring internal fixation or treatment with a halo, brace, or rigid collar. The following injuries were labeled a priori as clinically unimportant: isolated osteophyte avulsion fracture, isolated transverse process fracture not involving a facet joint, isolated spinous process fracture not involving lamina or simple compression fracture involving less than 25% of vertebral body height. Interpreting radiologists were blinded to the nurses CCSR results. Since only 47% of subjects had imaging of the cervical spine performed, investigators monitored each ED’s patient logs for 30 days to identify return visits by those with missed injuries because they did not undergo imaging at their original visit.
Results
From 4739 eligible patients presenting to the six EDs during the study period, 191 triage nurses enrolled 3633 patients. The triage nurses were predominately female (79.6%) with a mean 11 years working in the ED, and 29% had a baccalaureate degree. The patients were age 16 to 100-years with 74% arriving by ambulance and 1.2% with clinically important cervical spine injuries. The most common abnormal finding for the CCSR was inability to rotate the neck (Table), but nurses did not evaluate range of motion for 5% of patients so investigators later classified these cases as “indeterminate” since the CCSR was not actually applied. Nonetheless, nurses reported that they were very comfortable in applying the rule in 1681 cases (52.5%), comfortable in 1196 cases (37
.4%), neutral in 168 cases (5.3%), uncomfortable in 122 cases (3.8%), and very uncomfortable in 32 cases (1%) with similar responses across all six hospitals. All of the false-negative CCSR interpretations occurred in the first few months of the study.
Investigators also assessed interobserver agreement for the elements of the CCSR in 14% of subjects. Kappa, a measurement of agreement above that expected by chance alone, is reported for each component of the CCSR in the Table. If two nurses were to assess the same patient for the mechanism of injury, for example, we would expect that they would correctly label this CCSR risk factor as “present” or “absent” in 80% of cases above the agreement that they would have simply by chance (flip of a coin) alone.
As reported by investigators, the diagnostic accuracy for the CCSR in the hands of triage nurses was sensitivity 90.2% (95% CI 76%-95%), specificity 43.9% (95% CI 42%-46%), positive likelihood ratio 1.6 (95% CI 1.4-1.7), and negative likelihood ratio 0.22 (95% CI 0.09-0.51). The CCSR was “low-risk” (negative) for 1480 (40.7%) patients so spine immobilization could have been safely removed in triage if the rule had been applied.
Caveats
The CCSR cannot be used in children or in adult patients with GCS < 15, in uncooperative patients, or in those with known vertebral disease. In addition, the investigators reported that 99 patients had “indeterminate” CCSR results because triage nurses did not assess adequate neck rotation. Since the investigators excluded these subjects from their analysis of CCSR accuracy, readers cannot be certain as to the impact these cases would have on test reliability and should have reported a sensitivity analysis including best-case and worst-case scenarios for these “indeterminate” cases. In the worst-case scenario, one assumes that all of those “indeterminate” subjects with a cervical spine injury would have had a false-negative CCSR interpretation and all of those without a spine injury would have had a false-positive CCSR interpretation by triage nurses. Recalculating the diagnostic accuracy with these assumptions would yield a sensitivity, specificity, positive LR, and negative LR of 88%, 43%, 1.5, and 0.28.
Nobody contests that the malpractice environment in Canada and the U.S. are vastly different. Would a CCSR-labeled “clinically insignificant” spine injury without any operative intervention or long-term consequences increase an EP’s risk in court? Not surprisingly, recent survey data suggests that compared with other industrial nations, a U.S. physician is less likely to incorporate validated clinical decision aids into their practice. However, the standard of care for definitive evaluation of C-spine injuries is shifting towards CT and this imaging modality poses an increased long-term safety risk to our patients.
Nurses generally advocate for an expanded scope of practice in triage. Amongst physicians the best predictors of whether the CCSR will be used are exposure to the instrument in training and perceptions of difficulty incorporating the decision aid into clinical care. However, the current trial was strictly a validation trial. Triage nurses did not actually act upon their CCSR interpretations. While we await an impact analysis trial (where nurses are randomized to use or not use the CCSR to actually clear patients’ C-spines), ED leaders need to carefully weigh the risks versus benefits of devoting valuable resources to training triage nurses to more rapidly evaluate blunt neck trauma patients. One important implication of the current research is that nurse performance with the CCSR must be monitored early with continuing education provided probably focusing on the definition of high-risk injury mechanisms. Hopefully, future research will assess whether heterogeneous nurses can use the CCSR (or perhaps extrapolate these findings to the NEXUS) to decrease unnecessary imaging requirements, decrease overall ED length of stay, and improve other patient-centric outcomes.
Case Outcome
You decide that the Ottawa data is compelling, but not feasible to implement in the middle of the night so you file this data away with a commitment to develop a similar nursing educational initiative at your next department meeting.




3 Comments
I am becoming a doctor. Does the same standard apply?
If a nurse can do it, why not train the EMS system to do it and avoid the over-triage to the ED that constipates the waiting room in the first place? In most community hospitals, half the rear-end MVC patients need a grandmother more than a doctor.
Great idea. The same investigators who evaluated nursing C-spine clearance are now studying pre-hospital C-spine clearance (see http://pmid.us/21284880). Stay tuned!