Low-risk techniques to bring relief to this common complaint.
A 52-year-old Caucasian female presents to the ED with intractable neck/shoulder pain and tingling down the left arm. Her physical exam is significant for slight weakness in left wrist extension. She denies trauma and the pain has persisted since she awoke with it one week ago despite icing her neck several times a day.
Background
Cervical Radiculopathy (CR) is a complaint commonly seen in the ED with an incidence of 107.3/100,000 (men) and 63.5/100,000 (women), however a 2000-2009 military study identifying all servicemen diagnosed with CR illustrated higher incidence [1,5]. The North American Spine Society defines CR as “a pain in a radicular pattern in one or both upper extremities related to compression and/or irritation of one or more cervical roots.” [3] CR peaks in patients 50-54 years old, and risk factors include white race, female gender, cigarette smoking, axial load bearing, and prior lumbar radiculopathy [1].
CR frequently presents with pain in the neck that radiates to the trapezius and interscapular regions and may include concomitant motor, sensory, and reflex deficits. Presenting symptoms vary, and the picture may be complicated because the symptoms don’t always follow a dermatome or myotome distribution. Although symptoms can be debilitating, prognosis is generally good with 90% of patients seeing improvement with conservative treatment [3].
Etiology
Cervical radiculopathy most commonly involves C6 and C7 nerve roots. Cervical nerve roots exit above their corresponding pedicles (except C8) ventrolaterally through the neuroforamen which makes them vulnerable to injury. Spondylosis and disk degeneration leading to foraminal narrowing (70-75%) and herniated nucleus pulposus (22%) are the more common pathologies for non-traumatic mechanical compression [3]. Local ischemic effects and the inflammatory cascade play a large role in the natural progression of the condition through activation of a pathway triggering pain via sensitization of the nociceptive fibers.
Differential Diagnosis
The differential diagnosis for neck and shoulder pain, numbness, and tingling is extensive and includes many non-neurologic causes (Table 1). As health providers, it is critical to identify the symptoms that differentiate CR from life-threatening and infectious diagnoses. A thorough history and physical is often sufficient to rule out need for further workup. For instance, focal deficits of CR can mimic CVA symptoms. When lower extremity symptoms, CN deficits, gait and speech disturbances, or marked loss of strength are present, it should prompt workup with CT or MRI of the brain to assess ischemia or infarct.

Making the Diagnosis
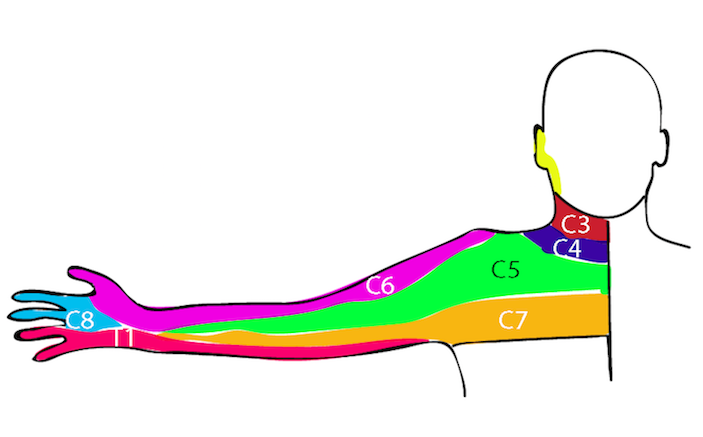
Neurologic findings that correlate with dermatomes have been found to correspond with pathology found during surgery [1]. Figure 1 corresponds the nerve root distribution to manifesting symptoms.

There is no single test with sufficiently high sensitivity and specificity, but a recent analysis describes 5 techniques to help discern cervical radiculopathy from its differential diagnoses (Table 2) [4].

Imaging is largely non-specific in the diagnosis of CR and should be ordered thoughtfully given high rates of false-positive findings [1]. When red flag symptoms are present (Table 1), MRI should be considered to rule out serious infection or neurosurgical emergency. X-ray and CT can identify bony alignment issues, but radiographic degenerative findings may not necessarily be the cause of a patient’s symptoms [5]. Outpatient EMG (sensitivity 50-71%) can be used in adjunct to other tests if needed [5].
Osteopathic Manipulation In The ED
Providers familiar with osteopathic manipulation may find it useful to treat patients with non-traumatic CR. The following low-risk techniques aim to increase the intervertebral space, widen cervical neural foramina, and reduce inter-disc pressure [6]. General consensus is to discourage cervical extension in CR. This succession of gentle modalities should take under four minutes. If the patient does not tolerate a technique, reassess the amount of force being used and proceed to the next modality if poor tolerance persists.
A) Sub-Occipital Release: Provider places both hands’ fingertips on the base of the patient’s occiput and applies slow superior traction targeting the fascial tissue plane. A release of the fascia will be felt as this taut connective tissue gives way. An end-point will be palpated in 45-60 seconds.
B) Soft-Tissue: Take 30 seconds to massage the cervical paravertebral and trapezius muscles. Include muscles of other involved regions as the patient tolerates [6,7].
C) Cervical Traction: Contact points may include mastoid processes, occiput, occiput/chin, and occiput/forehead. Apply 45-60 seconds of gentle superior traction with mild cervical flexion [8].
 D) Muscle Energy (Figure 2): If restriction or symptom relief is noted with flexion and side bending, the provider can engage the planes being assessed until reaching an end-point.6 The patient gently counters the provider’s unyielding force for 3-5 seconds, then relaxes with a deep breath. Upon exhalation with continued relaxation, the provider re-engages the plane to the advanced end-point. Repeat 3-5 times ending with a final stretch.
D) Muscle Energy (Figure 2): If restriction or symptom relief is noted with flexion and side bending, the provider can engage the planes being assessed until reaching an end-point.6 The patient gently counters the provider’s unyielding force for 3-5 seconds, then relaxes with a deep breath. Upon exhalation with continued relaxation, the provider re-engages the plane to the advanced end-point. Repeat 3-5 times ending with a final stretch.
Treatment
When debilitating symptoms are absent, conservative treatment may be initiated in nearly every patient. Cochrane reviews and the International Association for the Study of Pain list NSAIDs or oral steroids, Gabapentin, Nortriptyline, SNRIs, and muscle relaxants as useful first-line agents, with opioids and tramadol as second-line for the treatment of CR [3].
While short term immobilization and rest may calm symptoms of CR, a recent literature review showed that exercise is beneficial for improving function and activity levels of patients based on the International Classification of Functioning, Disability and Health.9 Patients with a history of CR have been found to demonstrate poor endurance and greater fatigue of the cervical muscles [10]. Thus, exercise programs for patients with CR aim to restore normal posture, mobility, and strength in the cervical spine and resolve symptoms more quickly [10]. Since it is often several weeks before an ED patient can obtain a PT evaluation, initiation of simple therapy upon discharge may bring relief and accelerate healing. The following are simple PT exercises that can be demonstrated by providers and offer the greatest benefit to patients.
Shoulder Circles
Goal: Reduce pain caused by spasm of the cervical extensors and upper trapezius muscles. Instructions: Rotate the shoulder blade one arm at a time in a circular fashion by elevating, then retracting, protracting, and re-elevating the scapula to complete the circle. Encourage patients to exaggerate the motion, moving the scapula as much as possible in all directions using the muscles of the upper back and neck while keeping the arm relaxed. 25 repetitions forward/25 backward BID.

Postural Stretching /Scapular Strengthening Exercises
Goal: Reduce the negative effects of kyphosis and forward head position which is common among patients with CR. Instructi ons: Gently stretch the pectoralis minor by stretching through a doorway while actively retracting the scapulae by engaging the scapular muscles (Figure 3). Position the head with the chin level and cervical spine in slight retraction. Hold 10-15 secs, 10 repetitions each BID.

Cervical Range of Motion Exercise
Goal: Relieve spasm by stretching the cervical musculature. Instructions: Reach over the top of the head with the contralateral, pain-free arm, gently pulling the head until a mild stretch is felt in the upper trapezius and lateral musculature of the cervical spine (Figure 4). Hold 10-15 secs, 10 repetitions each BID.
 Upper Back and Cervical Strength Exercise
Upper Back and Cervical Strength Exercise
Goal: Restore normal cervical lordosis and proper position of the head. Instructions: Use his/her hand or a towel to provide isometric resistance to muscles that support the cervical spine and head. The patient contracts the cervical muscles to resist the force created by pushing with the hand against the symptomatic side such that no motion occurs at the neck. The patient should be instructed to resist the motion of lateral flexion while actively retracting the shoulder blades (Figure 5). Hold 7 sec, 15 repetitions each for 2 sets daily.
Steroid injections can be considered in patients who have failed conservative therapy and PT, although the risks and technical difficulty of the injection (complication rates as high as 16.8%) have steered many specialists away from this modality [1]. Surgical intervention shows clear benefit (90% of patients have improvement at long-term follow-up), but the long-term results comparing surgical and non-surgical intervention do not differ [5]. Therefore, conservative management for 6-8 weeks should be attempted prior to surgical intervention. Consider a referral between 4-8 weeks following onset of symptoms as there may be better outcomes in patients who undergo surgical intervention within 3 months of symptom onset [2].
The Case
After being discharged with NSAIDs TID for 10 days and home PT exercises, the patient’s symptoms greatly improved after 2 weeks. She was referred to PT for further care and experienced complete resolution of symptoms in 5 weeks.
REFERENCES
- Caridi, JM, et al. (2011). Cervical Radiculopathy: A Review. Hospital for Special Surgery. 7; 3: 265-272.
- Alentado, VJ, et al. (2014). Optimal Duration of Conservative Management Prior to Surgery for Cervical and Lumbar Radiculopathy: A Literature Review. Global Spine Journal. 4; 4: 279-286.
- Onks, CA, Gregory, B (2013). Evaluation and Treatment of Cervical Radiculopathy. Primary Care: Clinics in Office Practice. 40; 4: 837-848.
- Rubinstein, SM, et al. (2007). A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. European Spine Journal. 16; 3: 307-319.
- Woods, B., Hilibrand, A (2015). Cervical Radiculopathy: Epidemiology, Etiology, Diagnosis and Treatment. Journal of Spine Disorders & Techniques. 28; 5: E251-259.
- Boyles, R, et al. (2011). Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. Journal of Manual & Manipulative Therapy. 19; 3: 135-142.
- McReynolds, TM, Sheridan, BJ (2005). Intramuscular ketorolac versus osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. Journal of American Osteopathic Association. 105; 2: 57-68.
- Savaa, C., et al. (2016). Effectiveness of Neural Mobilization with Intermittent Cervical Traction in the Management of Cervical Radiculopathy: A Randomized Controlled Trial. DOI: 10.1016/j.ijosm.2016.04.002.
- Cheng, C.H, et al. (2015). Exercise Training for Non-operative and Operative Patients with Cervical Radiculopathy: a Literature Review. J.Phys Ther Sci. 27; 9:3011-8.
- Halvosen M, et al. (2014). Endurance and Fatigue Characteristics in the Neck Muscles During Sub-maximal Isometric Test in Patients with Cervical Radiculopathy: Eur spine J. Mar;23; 3: 590-8.



4 Comments
Thank you for this outstanding review of a very common ED compliant. The pictures, diagrams and text throughly encapsulated all you need to know. I especially appreciated the Osteopathic Manipulation in the ED section, as a practicioner who does this daily, it is nice to know I am not alone and perhaps encourage others to treat instead of just medicate! I am sharing this article with my entire group.
Had surgery for injury to c-5-6-7 had problems in right arm. Some has subsided but now I’m having wrist and midrange, upperarm and pain from left shoulder neck going down. coming from c-6-7 had surgery but now this what can I do to relieve some of this pain. Already Taking gabapentin and tramadol I don’t know what else to do is there any exercises that I can help relieve some of this pain that I am having I already take gabapentin 800mg 4xaday and And tramadol 50 mg 2x4times a day I’ve had prior back surgeries that’s why I’m taking gabapentin bath and tramadol’s but these are helping with the pain in my arm neck and shoulder is there any exercise that I can help do this or will this be something that I will have to live with tramadol’s
Excellent Article! As a Physiotherapist I found this to be a very concise, accurate and up-to-date summary of this condition with its variety of presentations and possible treatments.
Thanks for sharing!
Thanks for sharing such a nice article. The article is easy to understand and very informative. Keep sharing!