An estimated six million people in the U.S. have been diagnosed with AFib.[1] For many, the emergency room (ER) physician is often the first person diagnosing and treating their condition.
AFib is the most common type of cardiac arrhythmia,[2] and the role of the ER physician is critical to ensuring patients are set up on the proper treatment path. The key to improving outcomes for AFib patients is a timely referral to an electrophysiologist (EP).[3]
Approximately one in three AFib patients are initially diagnosed in the ER with 66% of those visits resulting in hospitalization.[4],[5] Early treatment is critical to addressing the considerable disease burden imposed by AFib.[6] Quicker diagnosis in the ER and a faster referral to an EP helps improve patient outcomes because it allows patients to start treatment plans sooner. These plans may include oral anticoagulation drugs and antiarrhythmic drugs or a cardiac ablation procedure.
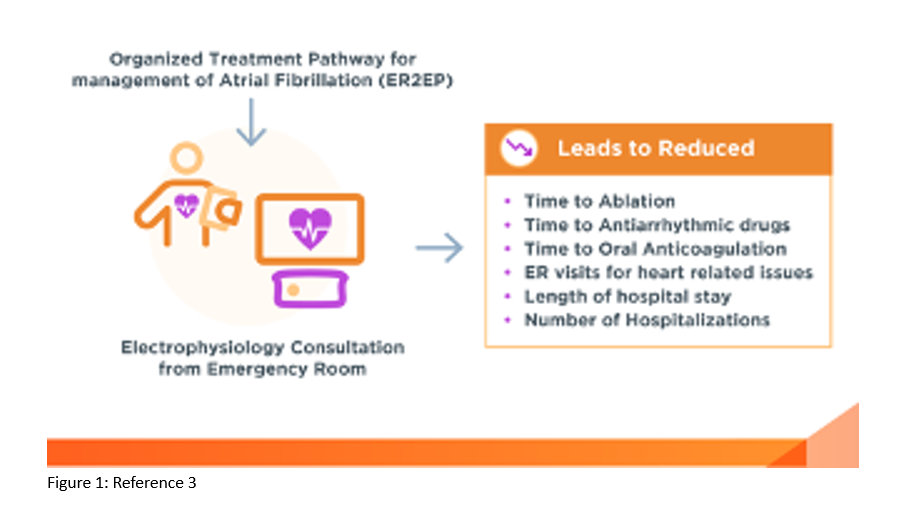
In addition to the health risks associated with delays in care, there’s also a significant cost burden. In fact, medical service utilization and costs are significantly higher among AFib patients than non-AFib patients. [6] A faster referral to an EP can reduce an AFib patients’ length of stay in hospitals, future ER visits for heart related issues and overall number of hospitalizations. [3]
Dr. Hakeem Ayinde is an electrophysiologist at Cardiology Associates of Fredericksburg in Virginia. By partnering with ER physicians and standardizing the referral protocol involving the EP service, his facility has improved access to care.
“Our team has an excellent working relationship with our ER staff,” explained Dr. Ayinde. “Being able to connect early with patients experiencing AFib allows us to provide better care and improve outcomes while also reducing time and cost. Our model of working closely with ER staff has made a positive impact on those we serve.”
AFib cases are rising and account for more than 450,000 hospitalizations annually.[7] Those seen in an ER and referred to an EP, either on call or soon after, tend to fair better than those who are not. [3]
By cutting out the delay in the hospital system and facilitating a patient’s access to an EP quickly, the amount of time to treatment could be reduced, which can in turn impact the morbidity and mortality that AFib imposes on lapses in care. [3] In fact, a study showed when emergency physicians secured early EP consults, the median time to evaluation by an EP was just one day, compared with 128 days for patients managed with routine protocol.[3]
One effective treatment option that an EP can offer to AFib patients is catheter ablation — a minimally invasive procedure that can restore a regular heartbeat. Despite the established evidence supporting the safety and effectiveness of catheter ablation procedures, currently only 5% of patients who could benefit from it get the procedure.[8]
Streamlining the pathway from ER to EP has shown to lead to much shorter times to catheter ablation (52.8 vs 180.6 days). [3] Studies have shown that drug refractory patients who have an ablation early to treat their AFib are likely to have better survival and less likely to revisit the ER or be hospitalized. [3]
“In our ER, we streamline patient consults with an EP to prepare a treatment plan as quickly and efficiently as possible. The sooner AFib is addressed, the better outcomes are for patients,” stated Dr. Ayinde.
As the prevalence of AFib increases, it’s becoming even more important to advocate for adapting an organized treatment pathway and prompt EP consultation for the management of AFib in the ER.
Creating an effective line of communication between the ER and the EP will help people experiencing AFib receive treatment sooner. This accelerated path can improve the overall health and wellbeing of patients by working to alleviate disease progression and allowing patients to live the lives they want. To learn more about how you can help your AFib patients, visit GetSmartAboutAFib.com.
US_BWI_ALLB_346864
© Biosense Webster, Inc. 2024
[1] Khavjou, Olga, D. Phelps, and A. Leib.“Projections of cardiovascular disease prevalence and costs: 2015–2035.” Dallas: American Heart Association (2016).
[2] Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. Int J Stroke. 2021 Feb;16(2):217-221. doi: 10.1177/1747493019897870. Epub 2020 Jan 19. Erratum in: Int J Stroke. 2020 Jan 28;1747493020905964. PMID: 31955707.
[3] Ahmed A., Garg G., Lakkireddy R.R. Impact of an Organized Treatment Pathway With Electrophysiology Emergency Room Consultation to Manage Atrial Fibrillation. American College of Cardiology. 2022 Sept 26.
[4] Hussein AA, Saliba WI, Barakat A, et al. Radiofrequency Ablation of Persistent Atrial Fibrillation: Diagnosis-to-Ablation Time, Markers of Pathways of Atrial Remodeling, and Outcomes. Circ Arrhythm Electrophysiol. 2016 Jan;9(1):e003669. doi: 10.1161/CIRCEP.115.003669. PMID: 26763227; PMCID: PMC5349298.
[5] Rozen G, Hosseini SM, Kaadan MI, et al. Emergency Department Visits for Atrial Fibrillation in the United States: Trends in Admission Rates and Economic Burden From 2007 to 2014. J Am Heart Assoc. 2018 Jul 20;7(15):e009024. doi: 10.1161/JAHA.118.009024. PMID: 30030215; PMCID: PMC6201465.
[6] Deshmukh A, Iglesias M, Khanna R, Beaulieu T. Healthcare utilization and costs associated with a diagnosis of incident atrial fibrillation. Heart Rhythm O2. 2022 Aug 4;3(5):577-586. doi: 10.1016/j.hroo.2022.07.010. PMID: 36340482; PMCID: PMC9626881.
[7] Tsao CW, Aday AW, Almarzooq ZI, et.al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation 2022;145:e153-e639. doi: 10.1161/CIR.0000000000001052.
[8] Internal Epidemiological Analysis.




1 Comment
The exposition on atrial fibrillation is very practical but succinct. I was hoping to see some pharmacological actions for the sudden and sometimes initial attack of atrial fibrillation.
Possibly many who read this do not have the necessary electrophysiological studies at hand, and perhaps an echocardiogram to identify cavitary thrombi, etc.
Thank you for the information
I have used google as a translator from Spanish.