“I think my child has swan flu!” You pause and try your hardest to maintain that poker face you’ve perfected. “I saw it on the news,” she continues, “and then my daughter was at Disney World running around with all these swans yesterday. I think they were contagious!” You’re still shaking your head as your resident comes up to you with her next case.
“I’m sorry to bother you, but the family in Room 8 really wants to leave. The father has an important meeting this afternoon, and he doesn’t want to wait for the contrast-enhanced KUB I ordered.” As your resident is handing the chart over to you to sign, you can feel the impatient eyes boring into the back of your head. The patient’s dad is standing at the doorway, arms crossed across his chest, with the typical “How long is this going to take?” look on his face.
His son, the patient in Room 8, has a complicated medical history and frequents your ED regularly for yanking out his G-tube. Although his stoma is fairly mature, and your resident was able to place a new Mickey without problems, you can’t help but think about a case you just read of online. A patient recently suffered disastrous complications from a tube feeding ended up in the peritoneum as a result of a misplaced G-tube. Your conservative inner voice tells you that you should still attempt to confirm placement with at least some type of imaging modality before sending them on their merry way.
Dad hovers over you as you explain to him that even though the risk for improper placement is small, you would still like to take a few steps to ensure that the new G-tube is sitting in the stomach. Unfortunately, you are unable to aspirate any gastric contents back, and you know it’s going to take at least an hour for the contrast KUB to get done. Before you can even utter the first word of your next suggestion, your resident chimes in, “I’ll go get the ultrasound machine. I think they are done using it in the trauma bay”.
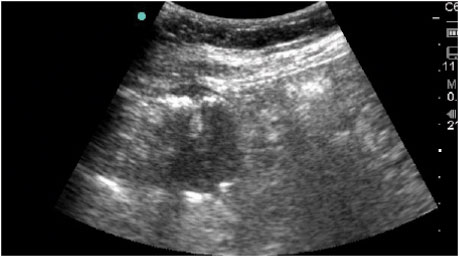
You apply some acoustic gel onto the skin just over the patient’s stomach and gently place the curvilinear probe just inferior to the newly placed G-tube. Scanning around, you find the muscular walls of the stomach and see gastric contents flowing in real time within the gastric walls.
You fan your probe cephalad and catch the following image. What do you see? See next page for conclusion.

As you scan through the stomach, you can see the balloon of the G-tube clearly within the stomach walls. You inject a small amount of normal saline into the G-tube lumen and watch on real-time ultrasound as the saline bubbles swirl within the gastric lumen. For educational purposes, you have your resident withdraw a bit of saline that is now mixed with gastric juices and ensure it’s acidic content with a quick dip of a pH strip.After using bedside ultrasound to help confirm proper G-tube placement, you feel better, Dad’s impressed by your sonographic skills and his short wait-time, and you and your resident can go back to practicing fast-food medicine where it’s “Your way and right away…”




1 Comment
Does anybody forego the ultrasound and just do the injfusion/withdrawal of some saline with ph testing to confirm placement? Is there any way you could get false reassurance if you had an appropriately acidic finding on the ph strip? (Just a medical student, be kind if I am missing something obvious)