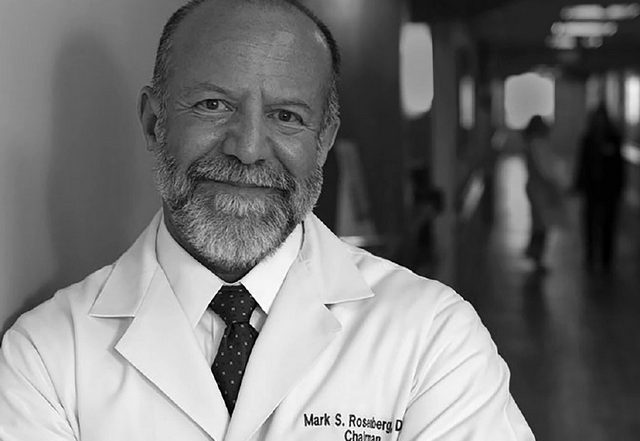
ACEP President Mark Rosenberg continues his discussion with EPM Editor-in-Chief Salim Rezaie, Board member Mike Silverman and Managing Editor Jeffrey Lyles as he details his ideas for patient volume, innovation strategies and the controlled chaos of emergency medicine.
SALIM REZAIE: We all know emergency medicine is not an easy job. It’s just not. It’s controlled chaos, as most of us like to call it. Now you have all these standards and regulations like: length of stay or door-to-doc time or all these check boxes; like you can’t eat at the workstation. The job’s hard enough and then there’s all these other things that seem to make it that much harder. What are those big hot topics and how do you plan on tackling those as ACEP president? I’d like to hear your thoughts on what you think are the biggest issues, stipulations, regulations that are making our jobs harder?
MARK ROSENBERG: Emergency medicine has put itself in a very interesting position. We straddle the fence in this hourly wage mentality. That’s how many of us were brought up. We want to be professionals, and yet we have more metrics to follow than anybody.
We need to look at all the structure that we consider appropriate from the beginning: like getting paid hourly, counting widgets [and]doing those things. But there is nobody else who controls emergency medicine more than us. This is our opportunity to really start looking. What I loved about COVID is it allowed for us to see the future more quickly. It showed us every crack in our system and how it stresses us.
So when my doc said to me: How come it’s so much harder now? Well, it is because you’re putting on PPE and you’re doing those things. But since COVID started in this past year, we’ve had more documentation requirements than we added on in any prior year. We’ve had more metrics and leapfrogs and this and that. So COVID just accelerated that crisis of what I believe is the most painful part of our specialty and that is counting widgets and using the electronic medical record. Take that away and I think we can live again a little bit more easily.
How do I do that? I don’t know. This is going to require an innovative task force to go back and look at some ideas and pilot them. And there’s probably some that are out there if we look at a climate survey for everything.
MIKE SILVERMAN: And I think that the well-being is in part balanced by the acuity that we’re seeing — the patient volume that we’re seeing. I don’t think that kind of magical two patients an hour that we’ve all kind of thought about is feasible in the current patient climate. Maybe there is a role for ACEP to go in there and kind of recalculate what a realistic patient per hour is now.
ROSENBERG: It really does come down to reimbursement. It does come down to policy because that really guides the business of emergency medicine, whether you want to call it a business or not. And those metrics are the ones that cause us the greatest angst for everything. I really think recalculating what our face is will take the pressure off a lot of those who say: I can’t get to two anymore. I can’t get to two more patients. What’s wrong? Let me push harder. And the pushing harder is each patient needs a certain amount of care. If we give each patient the care that they need, what’s the calculation?
REZAIE: What do you see being kind of some of the key issues in emergency medicine moving forward after we get out of this crisis?
ROSENBERG: Well, I think they’ve already started to evolve. We are in the beginning phases of starting an innovation center strategy at ACEP. So let me talk about the two think tanks that we have working now – Think Tank 1 and 2.
Think Tank 1, or innovation chamber 1, [has been assigned]highlighting current and future pandemics.
The second one’s huge and I’m super excited about it. Dr. Fauci said that our current crisis in America is health disparities when it comes to COVID. ACEP has always done a great job with diversity and inclusion. Our doors are always open and welcoming people 24/7/365, regardless of ability to pay. And we have been on the edge of the diversity leader in healthcare already.
We lead the initiative to help improve the healthcare of our communities and improve health equity 24/7/365. To make this work, we need a telemedicine, telehealth digital transformation task force because it can’t work without putting the pieces together.
REZAIE: I wanted to get your thoughts on risks and benefits of corporate emergency medicine and how we can help some of these independent groups continue to prosper and maybe even start seeing more of them across the country?
ROSENBERG: This a great question. And we’ve heard the council speak. There’s some bad business practices out there. I think there may be some bad small independent groups as well. This is emergency medicine and this is hospital-based medicine as we know it in 2020 and 2021. It makes money.
But let me go back 20 years and I have at that time a small, independent group I grew to several more hospitals. And every single day, my CEO would tell me what larger group came knocking on this door trying to steal my practice. At least my CEO told me. And I would call up my colleague, who owned his own group that has become a mega group, and I would say: What are you doing? He says: Well, it’s fair game. If they don’t like how you’re working, maybe they’d rather work with me.
And in those days, that’s the business. Your colleague, your friend, your neighbor, the guy who you went to the Scientific Assembly with is trying to steal your practice. And I thought it was pretty damn bad. And I hated it. And I hated every single one of my best friends who were stealing my practice.
So now what happens is those practices get some money because they’re making big money when they steal my practice. They’re getting some money and I do a good job, so they can’t steal my practice. So instead they want to buy me, and they’re willing to pay me a good market rate to buy me.
I can still argue with them and work independently. I can negotiate with them. And you know what? Many of my colleagues and friends who “sold out” to some of these larger groups, whether they were private independent groups making a lot of money are now privately independent or retired. It’s wonderful. That is the American way.
When I look at people who say their contract got terminated, we need to make sure we understand what a good contract is. Because if your contract has a termination clause, then if your employer doesn’t need you anymore and they can invoke the clause that you agreed to. So our opportunity is to help emergency physicians in small groups and in large groups have contracts that they understand and know what they’re living with.
There should always be due process. Every time somebody tells me they weren’t afforded due process, I say: Let me see your contract; and it says right here that you will leave if for no cause or for cause. So is this a big group issue? Is this a contract management issue? Is this the buyer beware and we’re not really doing a good job teaching everybody what’s in their contract? We can tell them: This is the pay rate and here’s the malpractice type.
So we are doing the work of the practice ownership analysis and it is in the early phases. And we’re going to try to look at a lot of different dynamics. What my CEO says to me is when my group or hospital employees cost more than the private equity group, they’re going to the private equity group. It’s dollars and cents for them. I have to continue to fight that.
But what I’m saying is this is so multi-factorial. And Mike, you said it, you worked for many different practice locations and many of those practice locations; maybe your income overall for the same job would have been the same even though you had different employment relationships. So this is not an easy answer. It’s an easier question than answer. And hopefully ACEP through this initiative [we will do a]full evaluation of: the good, the bad, the ugly of all practice ownership models. And then it will come back to council and we would decide.
We also have to identify terminology. I’m not sure what a contract management group is. So I can’t say that it’s good or bad because I don’t even know what it is. Was I a contract management group when I put my house up on a lien to open up my first contract and I hired doctors and I gave them a contract? I thought I was a pretty good guy.
REZAIE: If there’s somebody who’s interested in getting involved in leadership and getting involved with ACEP, what is the easiest way for them to go about doing that?
ROSENBERG: Well, I think there’s two or three easy steps: join. And step two is: get involved. And that’s an important one that I’m going to spend a moment to talk about. When I finished my training, my mentor said to me: Join ACEP for life. And I did. And he was right in so many different ways. It gave me my career. It gave me my colleagues. We are one community and that community comes together at ACEP.
Really the easiest way to get involved at the ACEP level is to join a section. There’s so many special interest groups, so many sections. And if you’re interested in pain and addiction or wellness or anything, those sections are an amazing place to start meeting people, start feeling the family, start getting more involved; and then the opportunity to get on the committees and to really grow with it. It becomes your family.
And if we can share my email (mrosenberg@acep.org) on this, so that people can reach out to me individually; I will personally introduce them toward the pathway if they have difficulties finding it.
REZAIE: Mark, thank you so much. I know you’re a busy guy, so we really do appreciate your time. So thank you so much for doing this. And I’m so glad to hear you’re getting over COVID. This world, this specialty would not be the same without you. So thank you so much.
ROSENBERG: Thanks my friends.



2 Comments
Let me give another spin on the sell out of EM. Dr. Rosenberg says this: “Many of my colleagues and friends who “sold out” to some of these larger groups, whether they were private independent groups making a lot of money are now privately independent or retired. It’s wonderful. That is the American way.” But this is not the way medical practice is supposed to work. In a profession the senior physicians don’t fund their retirement off the future fees of the next generation.
What exactly was sold here? Facilities, equipment, property? Nope, ED docs don’t own this stuff. The sale was the right to skim the FUTURE earnings of current residents and junior physicians. Private Equity debt financed these purchases and intends to recoup the buy out costs and to reap their needed 15-20% ROI by taking the earnings of ACEP members and other EM physicians. This, by the way, is prohibited fee-splitting wherein the EM docs are forced to give up a portion of their fee above fair market value for the right to see patients. So how can we say it is “wonderful” that Dr. Rosenberg’s friends and colleagues hugely increased their retirement nest egg at the expense of the next generation while forcing them into working for corporations that engage in fee splitting?
Thank you, Dr. McNamara!