While acute abdominal pain is a common presenting complaint in emergency departments, the diagnosis of acute appendicitis can be extremely difficult in young children, who may not have the classic findings that are typically seen in older patients.
While acute abdominal pain is a common presenting complaint in emergency departments, the diagnosis of acute appendicitis can be extremely difficult in young children, who may not have the classic findings that are typically seen in older patients.
Q.Are there any blood tests besides a peripheral white blood cell count that can help predict the severity of appendicitis?
A. In this study, C-reactive protein and procalcitonin were found to be useful indicators of the severity of appendicitis. Children with CRP greater than 3 mg/dL and/or PCT greater than 0.18 ng/mL were found to have a greater risk of complications
Citation: Gavela T, Cabeza B, Serrano A, Casado-Flores J.C-reactive protein and procalcitonin are predictors of the severity of acute appendicitis in children. Pediatr Emerg Care. 2012 May;28(5):416-9
OBJECTIVE: The aim of this study was to evaluate the use of procalcitonin (PCT) and C-reactive protein (CRP) on admission as predictors of the severity of appendicitis in children.
METHODS: This article prospectively studied 111 consecutive patients admitted with a diagnosis of acute appendicitis between July 2009 and February 2010 and recorded the following variables: age, sex, time since diagnosis, laboratory data, complications (abscess, intestinal obstruction), presence of hemodynamic instability, mortality, length of stay, and need for admission to the pediatric intensive care unit. Patients were divided into 2 groups according to the diagnosis confirmed during surgery (group 1, appendicitis; group 2, localized or generalized peritonitis).
RESULTS: Group 1 comprised 69 patients, and group 2 comprised 42 patients. Procalcitonin and CRP values were significantly lower in group 1 than in group 2 (0.15 vs 4.95 ng/mL [P < 0.001] and 3 vs 14.3 mg/dL [P < 0.001]). For a diagnosis of peritonitis, a PCT cutoff of 0.18 ng/mL gave a sensitivity of 97%, specificity of 80%, positive predictive value of 72%, and negative predictive value of 89.3%. The equivalent values for a CRP cutoff of 3 mg/dL were 95%, 74%, 68%, and 96.2%. Complications and the need for admission to the pediatric intensive care unit were more common in patients with peritonitis.
CONCLUSIONS: On admission, CRP and PCT predict the outcome of pediatric patients with appendicitis. Children with CRP greater than 3 mg/dL and/or PCT greater than 0.18 ng/mL have a greater risk of complications; thus, intervention should be early, and patients should be monitored closely
Q. Are there any specific risk factors in children that are predictive of a perforated appendicitis?
A. In this study, there was an overall perforation rate of 38.6%. Younger age, longer duration of abdominal pain, fever, muscle guarding, and elevated C-reactive protein level were significantly associated with a perforated appendicitis.
Citation: Hung MH, Lin LH, Chen DF.Clinical manifestations in children with ruptured appendicitis.Pediatr Emerg Care. 2012 May;28(5):433-5.
OBJECTIVES: Appendicitis is the most common abdominal condition leading to urgent surgery in children. With the goal of identifying signs and symptoms that will allow prompt diagnosis of rupture of the appendix and thus decrease associated morbidities, our aim was to determine factors associated with ruptured appendicitis in children diagnosed with appendicitis.
METHODS: The medical records of children aged 17 years or younger with a postoperative diagnosis of acute appendicitis treated at Cathay General Hospital, Taipei, Taiwan, from January 2002 and May 2009, were retrospectively reviewed. The patients were divided into with and without ruptured appendicitis.
RESULTS: Of the 228 patients, 140 had a postoperative pathological diagnosis of a nonperforated appendix, and 88 had a diagnosis of perforated appendix, resulting in a perforation rate of 38.6%. Younger age, longer duration of abdominal pain, fever, muscle guarding, and elevated C-reactive protein level were significantly associated with a perforated appendix.
CONCLUSIONS: Younger age, longer duration of abdominal pain, fever, muscle guarding, and elevated C-reactive protein level are significantly associated with a perforated appendix; these factors should be closely considered in the evaluation of individuals with suspected appendicitis
Q. Are there any clinical scoring systems that can help to improve the accuracy of diagnosing appendicitis in children?
A. Bhatt et al validated the Pediatric Appendicitis Score (PAS) and found it to be helpful in the evaluation of children with possible appendicitis. Scores of ≤4 help rule out appendicitis, while scores of ≥8 help predict appendicitis. Patients with a PAS of 5-7 may require further radiologic evaluation.
Citation: Bhatt M, Joseph L, Ducharme FM, Dougherty G, McGillivray D.Prospective validation of the pediatric appendicitis score in a Canadian pediatric emergency department.Acad Emerg Med. 2009 Jul;16(7):591-6. Epub 2009 Jun 22.
OBJECTIVES: Clinical scoring systems attempt to improve the diagnostic accuracy of pediatric appendicitis. The Pediatric Appendicitis Score (PAS) was the first score created specifically for children and showed excellent performance in the derivation study when administered by pediatric surgeons. The objective was to validate the score in a nonreferred population by emergency physicians (EPs).
METHODS: A convenience sample of children, 4-18 years old presenting to a pediatric emergency department (ED) with abdominal pain of less than 3 days’ duration and in whom the treating physician suspected appendicitis, was prospectively evaluated. Children who were nonverbal, had a previous appendectomy, or had chronic abdominal pathology were excluded. Score components (right lower quadrant and hop tenderness, anorexia, pyrexia, emesis, pain migration, leukocytosis, and neutrophilia) were collected on standardized forms by EPs who were blinded to the scoring system. Interobserver assessments were completed when possible. Appendicitis was defined as appendectomy with positive histology. Outcomes were ascertained by review of the pathology reports from the surgery specimens for children undergoing surgery and by telephone follow-up for children who were discharged home. Sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) were calculated. The overall performance of the score was assessed by a receiver operator characteristic (ROC) curve.
RESULTS: Of the enrolled children who met inclusion criteria (n = 246), 83 (34%) had pathology-proven appendicitis. Using the single cut-point suggested in the derivation study (PAS 5) resulted in an unacceptably high number of false positives (37.6%). The score’s performance improved when two cut-points were used. When children with a PAS of or=8 determined the need for appendectomy, the score’s specificity was 95.1% with a PPV of 85.2%. Using this strategy, the negative appendectomy rate would have been 8.8%, the missed appendicitis rate would have been 2.4%, and 41% of imaging investigations would have been avoided.
CONCLUSIONS: The PAS is a useful tool in the evaluation of children with possible appendicitis. Scores of ≤4 help rule out appendicitis, while scores of ≥8 help predict appendicitis. Patients with a PAS of 5-7 may
need further radiologic evaluation.
Q. With the fear of radiation becoming more prominent, are there any studies besides a CT scan that can help with the diagnosis of appendicitis in the event that an ultrasound is equivocal or fails to visualize the appendix?
A. Ultrafast 3-T MRI is being utilized at some sites to assist with the diagnosis of acute appendicitis. The advantage is that it does not require sedation (in the right age group) and does not require IV or oral contrast.
Citation: Johnson A, Filippi C, Andrews T et al. Ultrafast 3-T MRI in the Evaluation of Children With Acute Lower Abdominal Pain for the Detection of Appendicitis
OBJECTIVE. The purpose of this study is to evaluate the feasibility of ultrafast 3-T MRI in the evaluation of children with acute lower abdominal pain for the detection of appendicitis.
METHODS: Forty-two pediatric patients (30 girls and 12 boys; mean age, 11.5 years; age range, 4–17 years) with acute abdominal pain were prospectively studied. Ultrafast 3-T MRI was performed with a three-plane single-shot turbo spin-echo sequence and an axial T2-weighted turbo spin-echo sequence with fat suppression. All scans were performed without sedation or oral or IV contrast agent. Scan times were less than 8 minutes 45 seconds (median, 5 minutes 40 seconds). Patients underwent CT or ultrasound or both as a comparison study to the MRI examination. The MRI, CT, and ultrasound examinations were interpreted independently by four board-certified radiologists who were blinded to patient information, study interpretations, surgical pathologic findings, and final diagnosis.
RESULTS: Twelve of 42 cases of acute appendicitis were detected with 100% sensitivity, 99% specificity, 100% negative predictive value, and 98% positive predictive value, all of which were statistically significant (p< 0.01). The pooled and individual receiver operating characteristic curves for radiologists’ interpretation of the diagnosis of acute appendicitis were greater than 0.95 in all cases (p< 0.01)
CONCLUSION: Ultrafast 3-T MRI is a feasible alternative imaging modality for the diagnosis of acute appendicitis in children, particularly in cases where ultrasound is equivocal or nondiagnostic, as an alternative to CT. Ultrafast MRI requires no sedation and no oral or IV contrast agent and has no associated radiation exposure risks.

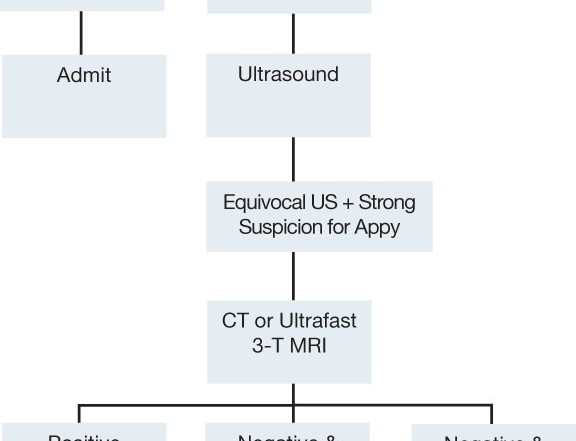
BOTTOM LINE: Since most sites do not have access to procalcitonin levels at this time, CRP is a useful adjunct in the diagnosis of acute appendicitis. A useful algorithm can be viewed above. In patients with an elevated WBC and CRP with a PAS score of ≥8, the child should be admitted to the surgical service. If the diagnosis is not as certain, an ultrasound in the hands of experienced operators and radiologists is the next step. If the US is positive, then the patient is admitted to the surgical service. In the event of an equivocal US, then either a CT or ultrafast 3-T MRI should be performed in patients in which the provider has a strong clinical suspicion for appendicitis. If these studies are negative and the patient is pain free, the patient can be discharged with close follow up. However, if the patient has persistent pain, the child should be admitted for observation. It is important to recognize that younger age, longer duration of abdominal pain, fever, muscle guarding, and elevated C-reactive protein level were significantly associated with a perforated appendicitis.



1 Comment
Diets, even the relatively healthy ones, are only short-term solutions to your weight or health problems.
My dad, who was having health issues, was encouraged by his doctor to change
his diet to basically all raw vegatable and fruits.
What have your experiences been with iridology
or change in the color of your eyes.