The otherwise healthy 27-year-old thinks it’s an abscess. Do you agree?
You are working Friday the 13th in the fast track area of your ED when you go in to see the first patient of your shift. He is a 27-year-old single male with no significant past medical history who is there for 4 days of gradually worsening pain and swelling in his right upper inner thigh. He says that the pain and swelling just keep slowly getting worse and he has no idea what it is because he’s never had anything like this before. He showed it to a friend who told him it is probably an abscess and that he should go to the ED to get it lanced. The patient denies any picking, pimple or other injury. He also denies any fever, dysuria, new sexual contacts, penile discharge, vomiting or other symptoms. He also denies any recent travel or exposure to animals that he can recall. He states he is really scared about having to have it cut open and asks if there any other options.
On review of his chart you see that all of his vital signs are within normal limits, but do take note that the temperature is 99.2, which is a little higher than you would expect. You also note that his pulse was 90 in triage and still is. This also seems a tad high for this fit appearing young man. On physical exam, he draws your attention to an area of swelling about the size of a grape that is about 3 inches below the inguinal ligament on the right. There is no visible skin surface lesion, but there is some faint overlying erythema. There is no definite fluctuance, but the area is tender. You think it may be a lymph node but note no nearby or distal infection.
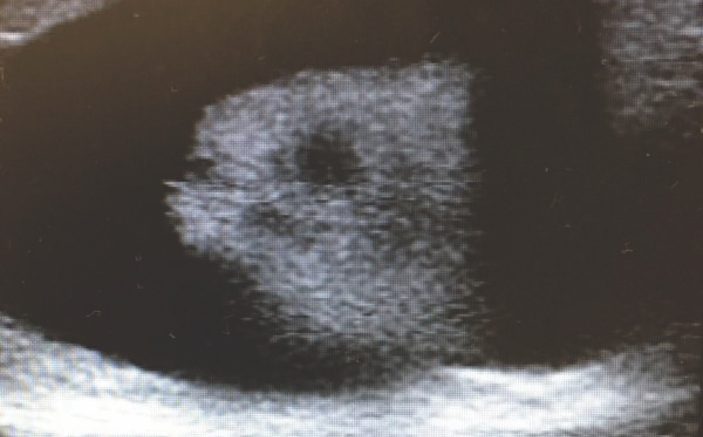
Since you are not entirely certain what you are dealing with, and the patient seems very apprehensive about scalpels and needles, you decide to take a look with the ultrasound. You obtain the image above. You then rotate the probe 90 degrees and the image appears about the same.
1. What type of structure are you most likely looking at?
2. What else might look like this?
3. What is the best next course of action?

1. What type of structure are you most likely looking at?
This is a swollen lymph node with an echogenic central medulla and an echo-lucent surrounding cortex.
2. What else might look like this?
A tendon with surrounding edema might look similar, but if you turn 90 degrees on the image it would look quite different. A blood vessel with a mobile DVT might also look like this, but would also look quite different if you turned 90 degrees. An abscess would not typically likely look like this.
3. What is the best next course of action?
Continue to search for a cause of the enlarged lymph node.

Discussion
Your bedside ultrasound shows a swollen inguinal lymph node about 3 cm in size with a fatty medullary core that is echogenic (white) and a surrounding near-fluid-density echo-lucent cortex (black). After obtaining this image, you wisely decide not to attempt incision and drainage or needle aspiration. Instead you attempt an often underused and underappreciated advanced medical procedure… a second history. A second, more focused history is often more useful than additional testing. I often teach residents that a second chest pain history is always required before a second troponin. There was no distal leg infection or symptoms or risks to suggest and STD so the patient was sent home on Keflex for presumed primary lymphadenitis, which is a condition that more commonly occurs in younger patients and in the neck rather than the groin. Fortunately he does well.
Pearls & Pitfalls: Soft Tissue Ultrasound
1. Probe & Positioning
Use a high frequency linear array transducer (10-13 MHz) for superficial structures and scans, such as soft tissue masses, in order to get more detail. Apply a large amount of ultrasound gel to improve your acoustic interface. For very superficial structures use a stand-off pad (you can improvise with a bag of saline) or, if feasible, water immersion.
2. Target Confirmation
To avoid a case of mistaken identity, always obtain images in multiple planes (longitudinal, transverse, oblique). This helps determine if a structure is spherical or elliptical like an abscess, tubular like a vessel or elongated like a tendon or nerve. In addition, always utilize a contralateral side for comparison whenever possible.
3. Cellulitis or Abscess?
Ultrasound can be used to help delineate whether a patient has cellulitis alone or a concomitant underlying abscess and to identify the size and depth of any fluid collection. Start by scanning normal tissue margins surrounding the area of interest. Normal subcutaneous tissue will have dark, hypoechoic regions of fat mixed in with brightly hyperechoic muscle, facial, and tendon planes. Cellulitis will demonstrate cobblestone edema. An abscess will show a spherical or elliptical collection of hypoechoic or heterogeneous material. While scanning, also try to identify nearby nerves, blood vessels and other structures to help prevent accidental damage during any planned procedure.
4. Necrotizing Fasciitis
One should always consider the worst possibility in an ED patient. For soft tissue infections this would be Nec-fasc and ultrasound may be able to help at the bedside by identifying gas formation. Since pockets of gas reflect sound waves they appear hyperechoic. They also can cause dirty acoustic posterior shadowing and far-field reverberation artifact. During your scan be on the lookout for these findings within the skin and underlying tissue and fascia.
5. Abscess Mimics
Pseudoaneurysms and large vessels may look like a fluid filled abscess on ultrasound. If you image in multiple planes, a vessel will appear as a cylinder but an abscess will remain egg-shaped. When in doubt, apply color-Doppler to the area of concern. Swollen lymph nodes can also mimic an abscess but usually have a hyperechoic central medulla and a hypoechoic outer cortex.
6. Practice, Practice, Practice
The best way to minimize errors is through experience, so scan lots of normal anatomy. The more scans you do, the better you will be able to differentiate abnormal from normal, even when you may not be sure exactly what the abnormality is. An image library of normal and abnormal scans helps immensely. Find mine at ERPocketBooks.com