Postcoital pelvic pain can turn into a specialist turf battle – but point-of-care ultrasound can help marshal resources and guide disposition
 A 25-year-old female presents to the ED with her boyfriend after she developed sudden onset pelvic pain during sexual intercourse at around 10 pm. The pain gradually worsened and spread to her ribs and she felt bloated and had the urge to defecate, so she got up from bed and went to the bathroom. Unfortunately she fainted on the way there, though she landed on carpet without injury. Her boyfriend had fallen asleep and woke when he heard her fall. He helped her to the bathroom but despite the strong urge to defecate she was unable to have a bowel movement. She then fainted a second time in his arms, so he brought her to the ED.
A 25-year-old female presents to the ED with her boyfriend after she developed sudden onset pelvic pain during sexual intercourse at around 10 pm. The pain gradually worsened and spread to her ribs and she felt bloated and had the urge to defecate, so she got up from bed and went to the bathroom. Unfortunately she fainted on the way there, though she landed on carpet without injury. Her boyfriend had fallen asleep and woke when he heard her fall. He helped her to the bathroom but despite the strong urge to defecate she was unable to have a bowel movement. She then fainted a second time in his arms, so he brought her to the ED.
She denies any significant pain or injury from the initial faint and fall, but continues to have pelvic pain, bloating, discomfort just below her ribs, tenesmus and light-headedness. She denies any fever, vomiting, diarrhea, vaginal discharge or bleeding or other symptoms. She states she is otherwise healthy, felt fine earlier today, and has never had problems with constipation or fainting in the past. She states she had a completely normal period about two weeks ago.
On physical exam she appears to be in mild distress with normal vital signs except for a pulse of 118 at triage, which is now down to 81. Her BP is 102/53, temperature 98.8 and respiratory rate is 19. Her abdomen does not appear enlarged but she states it is usually flatter than it is now and her boyfriend agrees. She has diffuse tenderness with diffuse guarding and possibly some mild rebound tenderness. The rest of the physical exam is essentially normal.
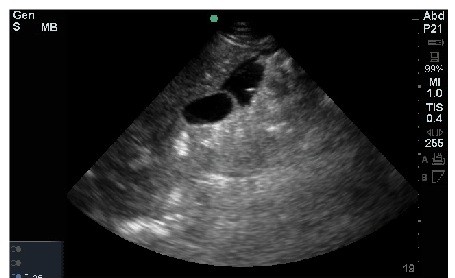
Worried about the possibility of a ruptured ectopic, despite the history of a normal period two weeks ago, you perform a bedside ultrasound of the abdomen and transabdominal ultrasound of the pelvis and obtain the following views (Images 1, 2 & 3). What do the images show? What should you do next?
What do the images show? What should you do next?
Dx: Hemoperitoneum

Image 1 is of Morrison’s pouch and shows free fluid. It is important to fan through and around Morrison’s pouch systematically as you may not always see free fluid on the view that best shows both the liver and the kidney. Though this is the view showed in most text books, if you stop there, you may miss free fluid nearby. Sometimes fluid is only seen at the inferior tip of the liver. In this patient the fluid was most prominent around the gallbladder. Image 2 is a little difficult to interpret. It is a sagittal view of the pelvis and shows clotted blood along with some free fluid in the lower pelvis. The bladder was empty as the patient had just urinated. This is not ideal for transabdominal pelvic imaging, but as you know, patients don’t typically prepare for their emergencies. In pelvic hemorrhage, it can be difficult to distinguish clotted blood from the uterus as they may have similar density. Take the time to practice ultrasounding the pelvis in normal patients. This will help you realize when things just don’t look right. Image 3 is a transverse view of the pelvis showing the “bow-tie” sign where the black fluid posterior to the uterus takes a shape similar to a bow-tie, or in this case perhaps racing goggles.
Given the history, exam, and bedside ultrasound findings you suspect she has hemoperitoneum either due to a ruptured ectopic or ruptured hemorrhagic ovarian cyst with ongoing bleeding. You page OB stat to the bedside. By the time the resident finishes her evaluation the labs are back. The hemoglobin is 10.2 and the pregnancy test is negative. The vital signs have remained stable although she is orthostatic. The resident confidently tells you, “Her whole abdomen is tender and she’s not pregnant; we don’t think this is gynecologic, and recommend you consult surgery.”
You’ve played with residents before and know they are usually motivated to try to turf ambiguous cases to other services. No one likes to take on extra work they won’t be paid for, right? Although you feel confident this resident is wrong you play nice and agree. You once did have a similar case in a young female that was actually caused by a ruptured splenic aneurysm, but in that case the onset wasn’t during intercourse! The surgical resident of course thinks this is a gynecologic issue and – you’re going to be shocked – recommends a CT of the abdomen to be certain. Another hour later – it would have been longer if you didn’t tell your charge nurse to put her at the front of the CT cue – the CT is read as free fluid in the abdomen and clotted blood in the pelvis with a probably adnexal source. The second hemoglobin is 9.1. You call back gynecology who – you guessed it – wants a formal pelvic ultrasound, which is what surprisingly both surgery and radiology both also recommended. The ultrasound shows – wait for it – clotted blood and free fluid in the pelvis and a probable ruptured hemorrhagic ovarian cyst. The third hemoglobin is 7.4.
The OB/GYN team finally agrees to admit her, but since her vitals are still stable, they want another hemoglobin level sent. The fourth hemoglobin is 5.9. They eventually transfuse two units and take her to the OR to stop the bleeding, which is what you tried to get them to do 4 hours ago, immediately after your bedside ultrasound, before the pregnancy test was even back and before she needed any blood. You’re glad she was never hypotensive. Or are you? Maybe it would have saved her a blood transfusion and shaved 4 hours off of your disposition.
Pearls & pitfalls to screen for Non-Traumatic Hemoperitoneum
1. Know When to Worry
The differential diagnosis for bloating includes the five “F’s”: Fat – no emergency, Flatus – no emergency unless it’s a bowel obstruction, Fetus – rule that out with a pregnancy test, Feces – no emergency, and Fluid. Fluid can be ascites, rarely urine from a bladder rupture, bowel contents from ruptured bowel, or blood. Bloating alone is rarely a red flag for anything serious, but when it occurs suddenly or is associated with severe pain, syncope or abnormal vital sign it can be a sign of non-traumatic hemoperitoneum. Other clues that the bloating might be due to something serious are pain radiating to either shoulder, pleuritic pain and tenesmus which can be due to compression of the rectum from clotted blood sitting in the pelvis.
2. Know the Causes
Trauma is not the only cause of a positive FAST exam. Ascites has many causes but is rarely sudden in onset. Bladder rupture rarely occurs in the absence of significant trauma. Causes of spontaneous hemoperitoneum may include the following: ruptured bleeding ovarian cyst, endometrioma, ectopic pregnancy, uterine rupture, AAA, splenic artery aneurysm, pancreatitis, ruptured hepatic cyst, ruptured neoplasm, DIC, and spontaneous splenic rupture.
3. Know What to Look For
Blood appears anechoic (black) when acute and free flowing, but hypoechoic (gray) when subacute or clotted. When blood is gray it is much easier to miss, especially if you are not looking for it or don’t know what it looks like. When there is clotted blood in the pelvis it will often make the ultrasound difficult to interpret and just look like a big mess. It may be difficult to identify the uterus. Always obtain multiple views and consider serial scans when a patient’s status changes. If something doesn’t look right, worry, even if you are not sure what it is.
4. Know a Few Tricks
The sensitivity of the FAST exam improves with Trendelenberg positioning, repeat imaging, and if you know how and where to look (experience). Always image the inferior tip of the liver, as this area may be positive when Morrison’s pouch is not. Likewise, blood can also accumulate near the inferior border of the spleen, even when the splenorenal recess appears normal. Turn down the gain on the pelvic view if the bladder is full, otherwise the enhancement behind the bladder may “white out” a small pocket of fluid. If you think you see a small sliver of free fluid, reposition the patient to see if the anechoic area changes or fluctuates. The sensitivity of the FAST for blood is ~85% if serial exams are performed, but it has been reported to be as low as 24% in some studies. Obviously the amount of fluid will affect sensitivity. Usually >200ml of fluid can be detected
5. Know the Pitfalls
The specificity of the FAST exam is about 95% (85% for > 200 cc of blood). False positives may include a variety fluid mimics that tend to by more hypoechoic (darker) that organs we are used to imaging like the kidneys, spleen and liver. These include the prostate, psoas muscle and perinephric fat pad. Larger than usual fluid filled organs can also lead you astray: severe hydronephrosis or a large blood vessel are two examples. Other serious causes of free fluid besides blood include urine and inflammatory fluid from infection, pancreatitis or ischemic bowel. Remember that it is beyond your scope of practice to rely on ultrasound to help you determine what type of fluid you see in the peritoneum. Bedside ultrasound should only be used to tell you whether or not free fluid is present. Always correlate your bedside ultrasound findings with the physical exam and clinical picture.
6. Practice Makes Perfect
With bedside ultrasound there is no substitute for experience. The more ultrasounds you do, the better you will be able to differentiate abnormal from normal, even when you may not be sure exactly what the abnormality is.



1 Comment
Image 1: Fluid at the Morrisons pouch.
2 & 3: Pseudogestational sac:
Stromgly Suggestive of Ruptured Ectopic.