In a recent issue of EM:RAP, Dr Michael Weinstock and colleagues review missed diagnoses, referencing a study by Kachalia et. al. They reviewed 122 closed malpractice claims from 4 liability insurers in which patients had an alleged missed or delayed diagnosis in the ED. A total of 79 claims (65%) involved ED diagnoses that harmed patients; 48% of these were associated with serious harm and 39% resulted in death.
In a recent issue of EM:RAP, Dr Michael Weinstock and colleagues review missed diagnoses, referencing a study by Kachalia et. al. They reviewed 122 closed malpractice claims from 4 liability insurers in which patients had an alleged missed or delayed diagnosis in the ED. A total of 79 claims (65%) involved ED diagnoses that harmed patients; 48% of these were associated with serious harm and 39% resulted in death.
The primary issues contributing to misdiagnoses were with the diagnostic process and with cognitive factors. Common issues with the diagnostic process were failure to order an appropriate diagnostic test (58%), failure to perform adequate history and physical (42%), incorrect interpretation of a diagnostic test (37%), and failure to order an appropriate consultation (33%). Ninety six percent of errors involved at least one of the following “cognitive” factors: mistake in judgment (87%), lack of technical competence or knowledge (58%), and lapses in vigilance or memory (41%). The cognitive factors contributed to almost every missed diagnosis but usually acted in concert with other types of factors, including handoffs, workload levels, and patient related factors. The authors conclude that the cause of missed diagnoses in the ED is complex, involving multiple process breakdowns and contributing factors.
Source: Ann Emerg Med. 2007;49:196-205
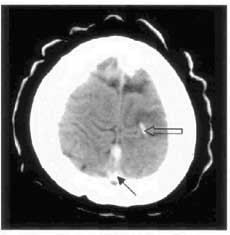
Dr David Williams presents a USC Grand Rounds talk on Cerebral Vein Thrombosis (CVT). When we first discovered this entity 160 years ago, mortality was uniformly 100%. After instituting heparin therapy in 1941, mortality has dropped to less than 10%. A CVT can simply be thought of as a DVT of the veins in the brain and has multiple infectious and non-infectious causes. There are three common presentations of CVT and key findings that help to distinguish it from other causes of headache. First, there is the stroke-like presentation with focal weakness. These patients may have an exam with a non-arterial distribution of weakness, or CT showing bilateral edema or hemorrhage. Patients may also present with seizure. The most common presentation is headache, occurring in more than 90% of patients. It can be gradual, over days, or sudden onset, mimicking subarachnoid hemorrhage. The presence of papilledema is an important finding and should be considered as part of the routine physical exam of the headache patient. The CT scan is normal in 30% of cases, but there are subtle clues that suggest the diagnosis. The “dense triangle sign,” (note: solid black arrow on CT) a dense triangle within the superior sagittal sinus from hyperdense thrombus and the “cord sign,” (note: open arrow on CT) a hyperintensity of the superficial cortical vein are both caused by thrombosed cerebral veins and can be visualized on a non-contrast head CT. The “empty  delta sign” is the converse of the dense triangle sign, which is only seen with the administration of intravenous contrast. The “cord sign” is considered pathognomonic for CVT. For definitive diagnosis, MRI with MRA and MRV adjuncts are the new gold standard. Treatment for CVT involves heparin anticoagulation and has shown beneficial effects in multiple studies, even in the setting of venous hemorrhage.
delta sign” is the converse of the dense triangle sign, which is only seen with the administration of intravenous contrast. The “cord sign” is considered pathognomonic for CVT. For definitive diagnosis, MRI with MRA and MRV adjuncts are the new gold standard. Treatment for CVT involves heparin anticoagulation and has shown beneficial effects in multiple studies, even in the setting of venous hemorrhage.
Source: David Williams MD; N Engl J Med 2005;352:1791-8; J Emerg Med 27 (2004), pp. 295–297
The ECG is one of the best tools for evaluating patients with syncope and, as Dr Amul Mattu points out, should probably be obtained in all such patients. In conjunction with the H & P, the 12-lead ECG is the “procedure of first choice” according to the American College of Cardiology and American Heart Association. The ECG should be evaluated for all of the following in all patients:
Dysrythmias: Bradycardia, atrioventricular block, intraventricular conduction abnormality, and tachydysrhythmias will not only provide a reason for the loss of consciousness but also guide early therapy and disposition of the syncope patient
WPW: Look for the short PR interval, delta wave and wide QRS. These patients can develop paroxysmal supraventricular tachycardia (PSVT, 70%), atrial fibrillation (25%), atrial flutter (5%), and, rarely, ventricular fibrillation. However, the delta wave will only be present if conduction is through the accessory pathway.
 Brugada syndrome: First described in 1992 as a set of electrocardiographic abnormalities associated with sudden death in otherwise healthy adults without structural heart disease. Although originally thought to be primarily a disease in men of Southeast Asian descent, more recent reports have noted the presence in women and children in most other areas of the world. The ECG abnormalities consist of a pseudo-RBBB pattern with ST segment elevation in the right precordial leads (V1/V2). These patients can then develop a polymorphic ventricular tachycardia, responsible for the patient’s syncope. This rhythm may also progress to ventricular fibrillation and cause sudden cardiac death. This diagnosis should be on the radar of every EP because it’s now believed to be responsible for 1 out of 20-25 cardiac arrests. Mortality is 10% per year, but if diagnosed early and treated with an AICD, mortality drops to 0%.
Brugada syndrome: First described in 1992 as a set of electrocardiographic abnormalities associated with sudden death in otherwise healthy adults without structural heart disease. Although originally thought to be primarily a disease in men of Southeast Asian descent, more recent reports have noted the presence in women and children in most other areas of the world. The ECG abnormalities consist of a pseudo-RBBB pattern with ST segment elevation in the right precordial leads (V1/V2). These patients can then develop a polymorphic ventricular tachycardia, responsible for the patient’s syncope. This rhythm may also progress to ventricular fibrillation and cause sudden cardiac death. This diagnosis should be on the radar of every EP because it’s now believed to be responsible for 1 out of 20-25 cardiac arrests. Mortality is 10% per year, but if diagnosed early and treated with an AICD, mortality drops to 0%.
Long QT syndrome: This syndrome can be congenital or acquired and is of main concern when the QTc> 500ms. These patients usually present in the first or second decade of life and may develop polymorphic VT, which can be precipitated by emotional stress or exercise. It is also important to note the causes of acquired prolonged QTC: hypokalemia, hypomagnesemia, hypocalcemia, Na+ channel blocking medications, and others (increased ICP, hypothermia, ACS).
Hypertrophic Cardiomyopathy: This genetic disorder affects 1 in 500 adults and although many patients remain asymptomatic throughout their lives, they may present with dyspnea, exercise intolerance, angina, syncope, and sudden death. The ECG is abnormal in 90% of patients with HCM, but the changes are usually non-specific. The most specific changes are the presence of deep Q waves in leads II, III, aVF, V5, and V6 in the early teenage years. These ECG changes may even precede the development of hypertrophy and echocardiographic abnormalities.
Source: Amal Mattu MD; American Journal of Emergency Medicine 2007; 25:688–701