Your local EMS will soon arrive with a spectator who had a witnessed cardiac arrest at a hockey game. Bystander CPR was immediately initiated but no onsite AED was available. On scene arrival, EMS found the patient to be in ventricular fibrillation (VF).
The Setup:
Your local EMS will soon arrive with a spectator who had a witnessed cardiac arrest at a hockey game. Bystander CPR was immediately initiated but no onsite AED was available. On scene arrival, EMS found the patient to be in ventricular fibrillation (VF). Two subsequent shocks restored a perfusing rhythm and restoration of a sustained blood pressure.
You note an obese gentleman in his late 30s. Vascular access is secured, and the patient is successfully intubated. He is maintaining a normal sinus rhythm with occasional PVCs. His twelve-lead EKG does not show any acute ischemic changes necessitating an urgent cardiac catheterization. He is stable throughout the period of ED assessment, but remains comatose without sedation being delivered either prehospital or in the ED. Two-hours later, your ICU colleagues are preparing to receive the patient as you prepare for shift change. Your oncoming ED colleague suggests initiating therapeutic hypothermia (TH).
The Choices:
1)Call your Critical Care physicians to ascertain what they think about post-cardiac arrest TH.
2)Tell your ED colleague that you’ve never heard anything so preposterous.
3)Push your patient’s gurney outside into the cold winter air and let the cooling begin.
4)Begin packing ice cubes under the axilla and groin while monitoring the patient’s body temperature.
The Question:
Does TH benefit cardiac arrest survivors when initiated in the ED immediately after resuscitation?
The Background:
Optimizing the otherwise poor outcomes of cardiac arrest survivors is a high priority for EPs. Obviously, the primary goal is preserving neurological outcomes in survivors not just admission to the ICU. As early as 1993, EP’s began contemplating TH as an alternative for cardiac arrest survivors after noting improved outcomes in victims of environmental hypothermia. Unfortunately, 75% (or more) of U.S. physicians have never used TH for cardiac arrest survivors (Abella 2005, Merchant 2006). Multiple clinical trials have now demonstrated variable degrees of benefit (survival with meaningful neurological outcomes) by using TH early in the post resuscitative course. Canadian Association of Emergency Physicians guidelines have addressed this issue with a number of recommendations for EM practitioners, but there is currently no similar statement from U.S. EM organizations.
The potential proposed benefits of TH include neuroprotection after anoxic no-flow states, inhibited activity of excitatory neurotransmitters, preservation of the blood-brain barrier, protection of ATP energy stores, reduction of damaging free-radical generation, decreasing raised intracranial pressure and increasing post-arrest cerebral blood flow. While it is currently impossible to prove which of these mechanisms contribute to better outcomes, one might reasonably assume that all play some part in maintaining neurological function.
The most conventional TH cooling methods include ice packs to the head/neck/axillae/torso/limbs, use of a cooling blanket or more invasive methods such as hemofiltration/dialysis. Central core temperatures are monitored with urinary, rectal or esophageal catheters. The speed at which cooling is achieved, duration of cooling and rewarming methods have been inconsistent from trial-to-trial.
Results:
This Cochrane review compiled all randomized trials prior to January 2007 examining the potential benefits of TH on cardiac arrest survivors. There were 4 trials and one research abstract study that enrolled a total of 481 patients included in the review. This review expands on a meta-analysis published in 2005, using individual patient data instead of aggregate study data. There were not enough studies to assess possible publication bias, and significant heterogeneity was noted in the cooling protocols used. The ultimate goal of a systematic review is to reduce uncertainty by comparing and combining different studies that assess the same intervention on similar populations. Since the objective is to understand the unique effect of the intervention-in-question upon the outcome of interest, one would not want to combine study results that compare different interventions in disimilar populations or using unrelated measurement tools. By measuring for heterogeneity, systematic review authors can quantitatively report whether differences between trials exceeded the differences one would expect by chance alone. If significant heterogeneity exists, then the systematic review authors should not combine the studies into a meta-analysis or they may be comparing apples and oranges (i.e. garbage-in = garbage-out). As with all Cochrane reviews, no industry funding was involved in writing this meta-analysis, and minimal biases were encountered in the included studies using the Cochrane Risk of Bias rating tools.
The primary outcomes were neurological status upon hospital discharge, survival to discharge and adverse event rates. The secondary outcomes included survival to 6 months or long-term (minimum 1 year) survival, degree of dependency for activities of daily living (ADLs) and cost-effectiveness of the TH intervention. Planned subgroup analyses, based on availability of individual patient data, included outcomes based on initial arrest rhythm, arrest location (in- vs. out-of-hospital), witnessed vs. nonwitnessed arrests and arrest cause (cardiac vs. noncardiac).
Neurological outcomes were defined using the cerebral performance categories (CPC) definitions as follows:
- Good CPC: alert, capable of normal life, may have functionally minor deficits.
- Moderate disability: conscious, alert, no dependence for activities of daily living (ADL). May be hemiplegic, ataxic, dysarthric, dysphasic, or have seizures and/or permanent memory problems.
- Severe disability: conscious/limited cognition. Dependence for ADL’s. May be paralyzed or severely cognitively impaired.
- Coma/vegetative state: not conscious/aware of external environment. No interactions (verbal/psychological) with environment.
- Certified brain death.
Authors grouped the outcomes into “good recovery” (CPC 1 or 2) or “unfavorable” (CPC 3-5).
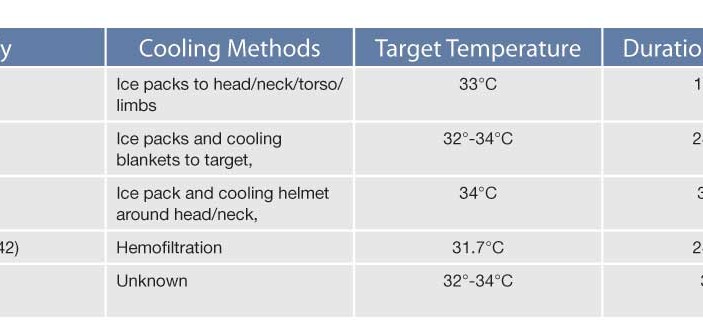
Three of the studies (195 cases/188 controls) employed conventional cooling methods such as ice-packs and cooling blankets (Table 1). This detail is important for discriminating readers to recognize since a number of more expensive intra-vascular or helmet-like cooling devices have emerged upon the market. Although these more expensive devices may one-day prove equivalent or superior to simple ice-packs, in 2010 there is insufficient data to support their purchase. Ice is readily available and it works, but carries the disadvantage of unintentional overc
ooling.
Bernard 2002, HACA 2002, Hachimi 2001, Laurent 2005, Mori 2000
For ice-pack cooling methods, there was a significant correlation between TH and good (CPC 1 or 2) neurological recovery and survival to hospital discharge (individual patient data; RR 1.55, 95%CI 1.22-1.96 and RR 1.35, 95%CI 1.10-1.65 respectively) translating to a NNT of 5 patients. The other two studies couldn’t be pooled since one used hemofiltration to achieve TH (no statistically significant difference), and the other (an abstract) did not specify cooling methods. Subgroup analyses showed better outcomes for patients who had a cardiac cause of arrest, out-of-hospital arrest, witnessed arrest or VF/VT as their initial rhythm. Cochrane did not report NNT’s for the subgroup analysis but BEEM has calculated them to report for EPM (Table 2).
No data was provided for 6-month (or longer) survival or for cost-effectiveness. No significant difference in adverse effects between the two treatment groups were noted, and no raw data was provided for event rates for the multitude of adverse events considered.
The Cochrane authors concluded that “conventional cooling methods to induce mild therapeutic hypothermia seem to improve survival and neurological outcome after cardiac arrest. Our review supports the current best medical practice as recommended by the International Resuscitation Guidelines.”
Caveats:
Survival from cardiac arrest with intact neurological status is a relatively rare phenomenon, and any intervention to maximize this possibility is worth considering. “Successfully” returning spontaneous circulation to a cardiac arrest patient with a suboptimal or horrendous neurological outcome is not in the best interests of patients, providers or society. For most EPs, interventions that maximize the opportunity to achieve a CPC 1-2 outcome would be optimal. The pooled study and individual patient data would suggest that TH is beneficial to achieve this clinical endpoint (NNT=5), especially in a situation of a witnessed out-of-hospital VF arrest of primary cardiac cause with spontaneous return of circulation.
TH is not risk-free (Dine 2009). Potential adverse effects include dysrhythmias (bradycardia, PVC’s, VF), metabolic (hypokalemia, hypocalcemia), hematologic (coagulopathy, thrombocytopenia, platelet dysfunction), and neurological (shivering, seizures). TH protocols are available online and courses are available to learn more about how to implement this new strategy into your post-resuscitation care.
The current data is insufficient to assess 6 month or long-term survival and economic outcomes. Furthermore, the benefits of intravascular cooling devices, helmets, or cooling vests remain to be determined. Certainly, ice packs are cheap and readily accessible in most EDs, and cooling blankets should also be available. The use of cooling helmets or hemofiltration may present more significant access barriers to implementation, but these were not the cooling method in the majority of studies. The ILCOR guidelines which advocate TH for post-cardiac arrest survivors are supported by this analysis of the research data.
Case Summary:
Using a cooling blanket and ice packs, you initiate TH for your survivor prior to his departure to the ICU. The ICU team takes the patient to the unit and initiates rewarming and extubation12-hours later. One-day later, the patient awoke and was subsequently discharged from the hospital a week later with only minimal memory and speech deficits.
The Bottom Line:
For witnessed out-of-hospital VF cardiac arrest survivors in the ED, cooling to a target core temperature of 32°–34°C is warranted. The Number Needed to Treat (NNT) to achieve a “good” neurological recovery is about 5 patients. The ideal duration of cooling and rewarming methods need to be delineated in future trials.
Suneel Upadhye, MD, MSc, FRCPC
Assistant Clinical Professor, Division of Emergency Medicine/Dept. of Clinical Epidemiology & Biostatistics, McMaster University
Christopher R. Carpenter, MD, MSc
Assistant Professor Division of Emergency Medicine, Director of Evidence Based Medicine, Washington University in St. Louis