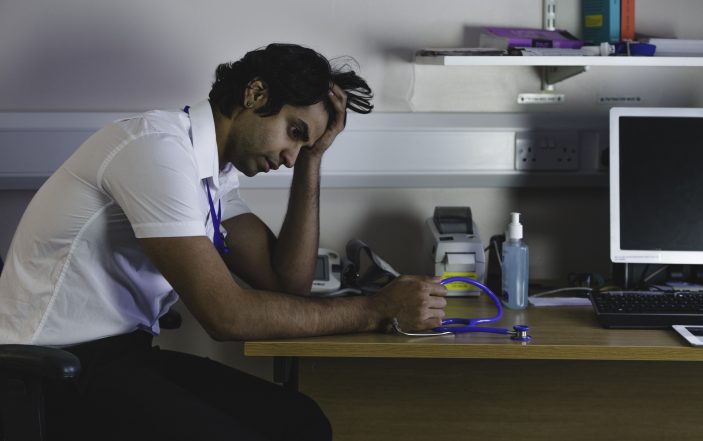
How to bring clarity to your thoughts and make your shifts easier.
Medicine is about decision making —especially in Emergency Medicine. Making difficult decisions based on imperfect information is one of the cardinal features of EM and the single most common reason that people leave EM for other specialties. In no other field of medicine do physicians and advanced practice providers have to make important and expensive choices based on very little information in a short period of time.
Making decisions is so automatic for most of us that we may not have realized how common or important this task is in our work day. Yet if you are like most people you have experienced the symptoms of cognitive fatigue, but may not have realized it. The purpose of this article is to identify when these symptoms are occurring and give tools that you can use both to prevent and treat the syndrome.
- Same chief complaint, different patient:
Experienced ED nurses will say that “it always comes in threes,” but in many EDs we can typically count on four or five or even more patients with chest pain or abdominal pain, and sometimes back pain or headache. When you have too many patients with the same complaints, it’s natural to lose track of details.
Signs and Symptoms: Decision fatigue can take a couple of different forms. One is getting the patients confused in your mind and making a mistake about where they fell on the decision tree for diagnostic studies and disposition. Another symptom would be thinking “I admitted the last patient with chest pain, I can’t admit this one too or the hospitalist will think I’m a sieve.” Or “I’ve CT scanned both the last two patients with belly pain, I should try not to scan this one.”
Treatment: To stop confusing patients, chart immediately after seeing the patient and refer to your notes before making your next decision. This does two things. It will clear your brain after you see the patient. Everything is written down, and you can press the reset button on your short-term memory and start the next patient on a clean slate. Then, when it comes time to decide whether to order additional testing or discharge the patient, review your notes so that the details are fresh. If you reread your note and find that you did not ask about pleurisy or shortness of breath, do so before you make your decision. Our decisions are too important to not be clear on the details. Lastly, remember that statistically the probability of an event is independent of prior events, so if you flip a coin and it is heads three times in a row; it is still 50/50 that it will be heads the next time. The same is true of your patient with chest pain or abdominal pain—it’s natural to try not to scan the third patient in a row, but don’t let prior decisions affect the way you care for the next patient.
- Decision overload
Feeling overwhelmed in a very busy day is a natural reaction. But like everything, it is how you react that separates the superstars from the docs that the nurses dread.
Signs and symptoms: Being indecisive, snappy or abrupt with patients, and putting off making decisions can all manifest when you feel swamped. Patient length of stays will increase disproportionally when decision making is impaired. However, when your department is busiest is when you need to be your best.
Treatment: Think about what you need most when you have a swamped ED: patient disposition. Then identify what you can do to help achieve that goal.
- Recognize that you are overloaded and do not give in to the temptation to put off decisions or procedures. Putting something off gives you a double burden: still needing to do it and also feeling internal pressure for not having done it already. The pelvic exam that is done weighs about four times less than the one that needs to be done. In addition, the information you obtain from the exam may allow you to disposition the patient by determining whether the patient needs a CT scan or can be discharged home.
- Message your nurses to limit interruptions. Ask them to use sticky notes or a white board for non-urgent communications. Interruptions are detrimental to safety and work flow at the best of times, and they are dangerous when you are already overloaded.
- Communicate your plan to the patient before you leave the room so that if you forget something they will remind you (“didn’t you say you were going to give me a tetanus shot?”).
- Don’t cut corners: double check drug dosages and do even simple math carefully.
- Lastly, documentation is important. You may not be able to get to the MDM, but always do the HPI and PE so you can refer to them when deciding on how to dispo the patient.
- Analysis paralysis
Signs and symptoms: Every so often I would come across a patient that I just couldn’t make up my mind how to manage. Looking back, my indecisiveness stemmed from a lack of sufficient information. Had I thought about it in those terms, I would have been able to pursue what information was needed to be comfortable making the decision. Instead, I would delay disposition until I had time “to think about it” or be forced to choose by the patient or the nurse.
Treatment: Crisp decision making is a learned skill, and it improves with experience. If you are new or just returning from time off, give yourself a break and simply ask yourself “what do I need to know to make a decision about this patient’s disposition?” Often, asking the patient more questions is the key. Don’t be afraid to “phone a friend”—your nurses, colleagues working with you that shift, or even an expert at your institution or another can all have helpful opinions. It is also fair to simply ask for tincture of time—a three-hour troponin, observation to see if a croupy child turns the corner or serial exams to determine if that abdominal pain may just be a smoldering appendicitis.
Summary: The world of emergency medicine revolves around making complex decisions that have big consequences over and over again. It is fatiguing, but is also a skill that can be developed and sharpened.
Much has been written on the topic, like Thinking, Fast and Slow by Daniel Kahneman, and “Getting Inside the Expert’s Head: An Analysis of Physician Cognitive Processes During Trauma Resuscitations” in the Annals of Emergency Medicine September 2018. It seems like an oxymoron to manage cognition cognitively, but doing so will bring clarity to your thoughts and make your shifts easier.