Emergency Medicine (EM) is a burgeoning medical specialty that is rapidly developing worldwide. Focused on the recognition, stabilization and treatment of life- and limb-threatening conditions, EM is established as a fully “mature” specialty in only a handful of nations, with 45+ countries in the early stages of development, including the Netherlands.
Abstract
Emergency Medicine (EM) is a burgeoning medical specialty that is rapidly developing worldwide. Focused on the recognition, stabilization and treatment of life- and limb-threatening conditions, EM is established as a fully “mature” specialty in only a handful of nations, with 45+ countries in the early stages of development, including the Netherlands. [Arnold, Smith, 2005; IFEM website] Nevertheless, in the Netherlands, emergency medicine (called spoedeisende hulp in Dutch—“quick, urgent help”) has developed at an intentionally quick pace, and has achieved many of the landmarks of EM development in just over 10 years. This article examines the development of EM in the Netherlands and elsewhere, and attempts to explain how regional-specific elements of emergency medicine development in the Netherlands embody a reasoned, deliberate approach to national development that can be used as a template for EM development strategies in the rest of Europe and the world.
The Need for Global EM development
Epidemiologic and demographic public health data reveal an already overwhelming need for Emergency Medicine (EM), trauma and acute care development. According to 2006 WHO studies on the Global Burden of Disease [WHO 2006], the worldwide forces of demographic and epidemiologic shift have elevated non-communicable diseases to the single largest cause of morbidity and mortality worldwide. The non-communicable diseases of trauma, cardiovascular disease, stroke and cancer have surpassed traditional communicable diseases as the major global causes of death for the first time in history. The so-called “diseases of Western Society” have become global, are increasing at a much faster pace than earlier anticipated, and in precisely those areas with the least-developed health care systems [WHO 2006].
Through first-hand and shared experiences in international medicine development, many in the IEM field have realized the difficulties and complexities of emergency medicine and acute care system development, and ensuring longevity of provision of high quality, affordable care. Collectively, the emerging discipline of international emergency medicine is learning that national and international medical development require expertise in many areas outside the field of medicine, and that any successful development of health care delivery systems, be it in emergency medicine or in other areas, requires extensive collaboration between the sometimes disconnected fields of clinical and academic medicine, administration and management, health economics, health law, health policy and public health.
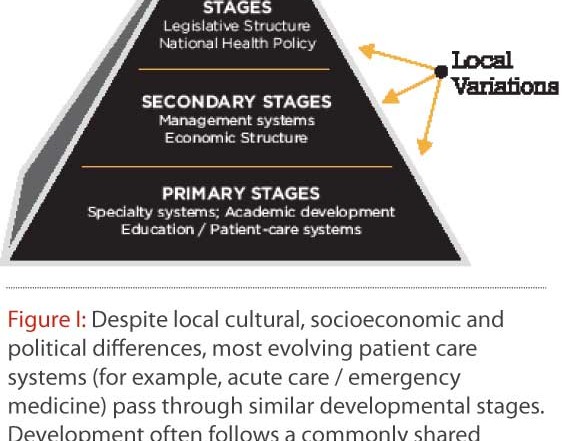
As study of the evolution of EM development in the USA has shown, and as extensive study of EM development in the 45+ other countries in the world where EM is currently in early or intermediate stages of development has reinforced, national and international EM development has (at least) 3 areas of focus:
Primary development: academic and clinical medicine (undergraduate, training and graduate physicians), patient care systems development, setting up residencies, teaching students and other health professionals, etc…
Secondary development: administrative and managerial training, financial and economic systems development, reimbursement, systems analysis, and
Tertiary development: health legislation, health policy and public health systems / agendas, patient safety, acute health care as a human right.
Over the short 10-15 year history of organized international emergency medicine development, most of our collaborations, projects and exchanges have focused on primary stages of EM Development. Until recently, this focus has been natural and well-reasoned: EM development depends heavily on the knowledge and skills of emergency physicians and other medical professionals, and on their ability to provide high-quality, focused care of acute patients.
In general, we have had much less collaboration and exchanges focusing on non-clinical secondary and tertiary stages of EM, despite evidence that these stages of development are often as important or more so than clinical and academic stages, especially as rate-limiting steps in mature EM system formation. Many new and emerging EM systems have focused solely or mostly on building the primary stages of EM in their systems, only to later encounter blockages and barriers to further development which might have been avoided if time had also been spent developing secondary and tertiary stages. For example, an examination of the mature EM systems from Canada to Singapore, as well as the quickly-maturing EM systems like Poland and Mexico, shows emergency medicine developing into the areas of EM administration and management, EM finance and health economics, health insurance expansions, emergency health care legislation, and public health.
This multi-level, multi-disciplinary approach is absolutely essential to ensure successful medical development, and to ensure program longevity, resilience and self-generation. EM development strategies should include training and development in each of these areas to facilitate capacity-building in local EM expertise.
Overview of International Emergency Medicine
“Among the most important factors affecting health system convergence are the dynamic character of medical knowledge and technology and the forces that sustain it; the effect of medical demand on national economies; changing demography and, particularly, the aging of populations; changing disease patterns; and increasingly rapid mass communication coupled with rising public expectations.”
[Mechanic and Rochefort, 1996]
Over the past twenty years, emergency physicians (EPs) have begun to examine the scope of EM and its extension into the fields of public health and primary care. Specifically, EPs have increasingly looked beyond their borders to learn how emergency medicine is practiced in other parts of the world. The emerging field of International Emergency Medicine (IEM) is concerned with the development of emergency medicine and acute care systems development in countries and regions where EM development is needed, and can be viewed as a subspecialty of EM; it allows emergency physicians and other health professionals who are involved in emergency medical care to learn from each other, and involves the education and training of emergency care providers throughout the world. [Rupke, 1993]
EM is established as a fully “mature” specialty in only a handful of nations, and another 45+ countries are in the early stages of development, including the Netherlands. In many underdeveloped and developing countries, the emergency medical care systems are much less established, with regional clinics, local general practitioners, nurses or other local healers providing the bulk of emergency medical and primary care. In more developed regions where hospitals provide primary, secondary and tertiary care, very often there is only a rudimentary emergency department, often staffed by under trained and inexperienced physicians, often with no dedicated 24-hour coverage of the emergency room, and rarely with emergency medicine specialty training. The EMS/prehospital system is highly variable, understaffed and underdeveloped, and there is in general vastly inadequate training for
emergency care providers, for doctors, nurses and medics alike. While the need for emergency medical care is as large or larger in these developing areas, too often these countries have inadequate or overwhelmed emergency medical care systems [Alagappan, Holliman, 2005].
In some regions, such as sub-Saharan Africa, EM is mistakenly seen as less pressing than more traditional primary health concerns such as infectious diseases, maternal and child health and other public health issues. In fact, EM can still play a role in underdeveloped regions in supplying acute episodic care and a much-needed link to the public health care system, as well as supply care for the emerging chronic diseases as depicted by the data supporting epidemiologic and demographic shifts.
Overview of Emergency Medicine in the Netherlands
In the Netherlands, emergency medicine does not yet exist as an official, fully-developed medical specialty. Health care delivery in the Netherlands is organized in a two-tiered system with a network of community-based general practitioners (GPs) providing primary care and acting as gatekeepers to hospital-based specialists. These GPs refer chronic problems to specialty clinics based in the hospital and acute problems to the emergency department for specialist consultation. Patients can also go to the emergency department on their own (self-referral). To date, of the 126 hospitals in the Netherlands, 106 have emergency departments (RIVM, 2007). As described by Elshove-Bolk, Mencl, Simons, et al in the European Journal of Emergency Medicine:
[These EDs] are staffed by loosely supervised interns and junior residents, without any specific training and are employed as emergency physicians. The specialists’ consults are also often conducted by loosely supervised residents, with varying degrees of training. It is these doctors who are responsible for the initial evaluation and treatment of the approximately two million patients treated in Dutch emergency departments annually.
[Elshove-Bolk, 2005]
Most patients presenting to emergency departments in The Netherlands are received by the most inexperienced young doctors: so-called artsen-neit-in-opleiding [doctors not in residency: first-year doctors waiting for residency opportunities elsewhere], together with older non-emergency residents in family practice, surgery and other specialties. This model of allowing the youngest, most inexperienced doctors tend to the sickest, most urgent patients is unfortunately not uncommon in most parts of the world, and is not particular to The Netherlands.
In recognition of this problem, in the 1990s, several Dutch medical professionals laid plans for training programs for emergency physicians in the Netherlands, and in 1999, the first national emergency medicine society was formed, the Nederlandse Vereniging van Spoedeisende Hulp Artsen. In 2003, the Stichting Opleiding Spoedeisende Geneeskunde was formed—the Foundation for Education in Emergency Medicine, which, until recently, acted as a certifying body of emergency medicine training programs. As of October 13, 2008, the Medical Specialist Review Committee (the national certifying body for new specialties) declared Emergency Medicine a “medical specialty profile”—a temporary intermediate-level specialty designation. Presently, there exist 16 accredited emergency medicine training programs in the Netherlands, with 10+ more currently in the process of obtaining accreditation. These programs have graduated approximately 120+ trained emergency physicians and approximately 150+ residents are currently in training.
EM Administration and Management Fellowships in The Netherlands
Currently, the training program for Spoedeisende Hulp artsen as recognized by the SOSG and the NL Board of Medical Specialists is only three years in length. This short training program length does not allow for full instruction in advanced, essential elements of clinical, academic, administrative, managerial and specialized areas of emergency medicine. During the presentation at the 1st NVSHA conference, I mentioned that I was in the process of formulating a 1-2 year post-residency “Fellowship” training program in administration and management in EM. Immediately after the lecture was over, I was pleased to notice that 20-30 individual EPs and residents came up to me to ask for more information on this Fellowship training program and how they could take part in it. From this initial outpouring of interest, I began to dedicate my time to designing a shorter Fellowship training program to meet the needs of this large group of Dutch emergency physicians.
To these ends, we developed the Administration and Management Fellowship in EM, which draws its rationale from the EM Development Pyramid concept illustrated above: that EM development needs to include more than just clinical and academic EM, and that emergency physicians in societies with newly developing EM systems need to gain training, expertise and experience in these areas.
Fellowship Overview
To date, the Administration and Management Fellowship in Emergency Medicine for emergency physicians and emergency medicine residents in the Netherlands has been run successfully three times, with 29 Dutch EPs having successfully completed the Fellowship, earning the designation of Fellow of the NVSHA (FNVSHA). This Fellowship Program has involved Dutch and international EM faculty and others, and has focused on a “train-the-trainer” model, where Fellows obtain both mastery levels of the course content, as well as specific instruction on how to conduct identical courses at their institutions. This teaching model has been very successful at disseminating the information presented to the Fellows by giving them reading, teaching and instruction materials to use and expand on their own. The Fellowships also focus on the production of individually-catered Fellowship Projects, which are specific, problem-oriented projects that Fellows bring back to their sponsoring institutions for immediate action and implementation. Past Fellowship Projects have included:
-the formulation of an EM curriculum for Dutch medical schools
-the development of an e-Portfolio for the newly released Dutch Curriculum in EM
-the formation of national quality indicators for Dutch EM (which were officially accepted by the Dutch Ministry of Health)
-investigations into formal feedback systems for EM education and practice
-the establishment of EM student organizations at every Dutch medical school.
On-going consultation by Dutch faculty, NVSHA and national and international faculty has been made available on-site, on-line and via telephone, and through advanced video telemedicine linkages before, during and after all forms of training.
The Fellowships have consisted of conferences, didactic lectures and academic teaching, reading and writing assignments and the completion of individual projects for each fellow.
Academic lectures, readings and didactic material:
The following areas are covered in conference, lecture, readings and other academic assignments:
-Administrative Principles in EM
-Management Principles in EM
-Hospital Management
-Academic and Training Principles in EM
-Patient Safety and Quality in Emergency Medicine
-Research in EM
-Development of the Specialty of EM
-Emergency Department Operations
-Health Economics, Policy and Law in EM Development
-Special Topics in EM (Global Burden of Disease, Acute Health Care as a Human Right, EM and Global Health Institute Consortia)
This is the first comprehensive international EM training program of its kind. While certain elements of our Fellowship have been taught in pieces for only the most advanced EM systems, our program is unique in that it is the first to bring together all of these requisite development topic areas into one training program, and is first in off
ering it to EPs working in developing and underdeveloped EM systems.
Interest in the non-clinical topics of Administration and Management and in this course has been large. The first Fellowship class in 2008 was extremely successful and prompted a second to follow in 2009, and then a third in 2010. Interest has also spread outside of The Netherlands. Our particular Fellowship course has been conducted in many places around the world, in developed, developing and underdeveloped regions alike. So far, in addition to the Netherlands, we’ve conducted region-specific courses in South Africa, Australia, Poland and Spain. We have plans for programs in Hong Kong, Botswana, the USA, Canada and elsewhere.
The European Society of Emergency Medicine has also validated the program, devoting three days to EM Administration and Management in the 5th Mediterranean EM Congress in Valencia, Spain in October 2009, and will sponsor a 3-day pre-conference on these topics at the EuSEM Congress this October 2010 in Stockholm, Sweden.
Many EM systems are struggling with these non-clinical aspects of EM development, and could benefit from concentrated training. There is a general lack of didactic material on the secondary and tertiary elements of EM development in nearly all national EM curricula, and a limited understanding of these traditionally non-medical areas by most physicians. Indeed, many of the international teaching faculty involved in our courses in The Netherlands have remarked about the conspicuous absence of such comprehensive, non-clinical training even for their own residents back home at their “mature” EM systems. It is one of the goals of this program for these non-clinical topics to formally be placed into national and international EM teaching curricula, and for the broader IEM community to become more involved in comprehensive EM development on many different levels.
 Future directions for emergency medicine in The Netherlands
Future directions for emergency medicine in The Netherlands
As described by Jeff Arnold in 1999, international EM development stages can be roughly divided into three major groups: underdeveloped, developing and mature. The so-called “mature” group includes the countries that many would consider having a fully-developed acute care system, such as the United States, Australia and Singapore. The “developing” group now includes 45+ countries that have officially recognized EM as a medical specialty but that are in various states of EM development.
In many aspects of its medical and health care system, The Netherlands is one of the best developed nations in the world. They lead the world in transplant medicine, genetic mapping, gene therapy and genomics, and hematology / oncology. They are even among the local European leaders in trauma care, prehospital care and critical care. However, for many historical, cultural, medical and political reasons, The Netherlands is arguably in the “developing” group with respect to its level of EM and acute care systems. It’s as if the Dutch health care system were a modern city skyline filled with skyscrapers, representing multiple areas of medical achievement and clinical excellence. In the middle of that impressive skyline sits a humble, four-story building representing the literal and comparative underdevelopment of EM and acute care delivery systems.
Among the 45 or so countries in this “developing” group, however, The Netherlands is emerging as one of the local leaders in national EM development in the EU community. In the short 10 years or so of Dutch EM development, they have achieved what has taken some other countries 30-40 years to develop.
In particular, the NVSHA development of the first Dutch national EM curriculum in 2006, now in its 2nd edition, is one of the most advanced and sophisticated national EM curricula so far, having studied and adopted the best pieces of the existing national EM curricula from Canada, the UK, Australia and the USA, and offering region-specific additions and improvements. This EM curriculum has proved to be one of the major influences on the structure and format of the EuSEM-authored “European Curriculum in Emergency Medicine” that was approved by the European Union of Medical Specialists in 2009. In addition, there is large and growing interest in more advanced EM development programs, such as the Administration and Management Fellowship, along with other EM teaching and development programs in Patient Safety, Medical Decision-Making, ED Design and EM Finance that are coming out of the EM development community in the Netherlands.
Through the elements in figure II and other examples, the EM community in The Netherlands is intentionally and deliberately addressing national EM development using particular focus on those EM development strategies that have been tried (with or without success) elsewhere. In this fashion, Dutch EM development is following templates for development as much as creating one.
By focusing on comprehensive EM development techniques, by concentrating on the EM development experiences of fellow countries and regions, and by gaining education and experience in multiple areas outside the field of medicine, The Netherlands is historically and politically well-positioned to offer its experience in successful EM development as a template for development outside its borders.
Conclusion
Emergency medicine is a new and expanding field in The Netherlands. Given the recent developmental steps that have taken place, the state of Dutch EM is growing and shows all prospects of flowering into full development in the near future. Further, the successes of EM development in The Netherlands will continue to spread to and influence EM systems in neighboring countries in the EU and elsewhere, and can be used as a guide and template for EM development abroad. As one of the “success stories” of goal-directed, intentional national EM development, The Netherlands has the opportunity to establish itself as one of the global leaders in national and international EM development.
REFERENCES
Arnold, J. International Emergency Medicine and the Recent Development of Emergency Medicine Worldwide. Ann Emerg Med. 1999;33(1):97-103.
Arnold, K, Smith J. Emergency Medicine Clinics of North America – International Emergency Medicine. Elsevier, 2005;23(1).
Elshove-Bolk J, Mencl F, van Rijswijck BT, et al. Emergency department patient characteristics: potential impact on emergency medicine residency programs in the Netherlands. Eur J Emerg Med. 2006;13(6):325-329.
The European Society of Emergency Medicine (EuSEM). www.eusem.org
International Federation for Emergency Medicine. www.ifem.cc
Holmes J. Emergency Medicine in the Netherlands. Emerg Med Australas. 2010;22(1):75-81.
Mechanic D, Rochefort D. Comparative Medical Systems. Annu Rev Sociol. 1996;22:239-70.
Nederlandse Vereniging van Spoedeisende Hulp Artsen [Dutch National EM Physicians Society] http://www.nvsha.nl
RIVM Rijksinstituut voor Volksgezondheid en Milieu [Dutch: National Institute for Public Health and the Environment.] http://www.rivm.nl/
Rupke John, ed. American College of Emergency Medicine: 25 years on the front line the ACEP anniversary 1968-1993 (Dulles: ACEP, 1993) 10.
SOSG: Stichting Opleiding Spoedeisende Geneeskunde [Dutch EM Certifying Body]. http://www.sosg.nl/
The World Health Report, 2006. (World Health Organization) http://www.who.int/whr/en/




1 Comment
please advise me on how i can get a space in your country/institution for residency in emergency medicine as a foreign student.