Discovering what lies beneath the scalp hematoma can be even trickier with an infant.
On a mid-afternoon shift, your upper-level resident presents a three-week-old female twin infant who was delivered at 33-weeks that was just seen in clinic 20 minutes ago for a well-check. She was sent to the emergency department to be evaluated for a head injury. Your resident is fairly unimpressed with the patient’s history of presenting illness and exam, as she explains that the patient accidentally fell off her maternal grandfather’s lap while he was attempting to feed the other twin sibling simultaneously.
The grandfather reports that he was sitting just about two feet from the ground when the patient fell. He is uncertain which part of the body struck the ground initially, but recalls that he was able to slide his foot under the patient in reaction just before she hit the hardwood floor.
Your resident proceeds with her plan based on the Pediatric Emergency Care Applied Research Network (PECARN) criteria in a less than two-year-old patient to monitor while patient is feeding and re-assess after your assessment is complete. The patient has already begun to start her next feed at the recommendation of the resident.
In considering other factors leading to the injury, a non-accidental trauma is low on your differential diagnosis as the story is also corroborated by clinic staff. On your exam, the patient appears well and is tolerating feeds. She is a little fussy when the bottle is removed during your exam, but easily consolable. You note a small erythematous patch on the left side of the scalp, but there is no edema or discomfort with palpation. The rest of your exam is normal, and you agree with the current plan.
Thirty minutes after the feeding, the patient still looks well, but you are called to bedside by your resident who reports a slight change in her exam.
“It feels like the the small bruise has gotten a little wider and bigger,” she says. “It’s very subtle, but different. What do you think?”
Your palpation of the scalp feels slightly softer than previously and the erythematous bruise is now a little darker. You explain to the family that given the change, you may consider getting a head CT recalling a recent lecture you heard from an ultrasound grand rounds on pediatric applications as an adjunct to patient care.
Taking into consideration that the patient looks clinically well, tolerating oral feeds with no signs or symptoms of a change in mental status and although the small bruise is located at the upper temporal and parietal scalp, you are not completely convinced that the patient needs a CT. So, you take the opportunity to attempt your newly acquired point-of-care ultrasound skill to examine the scalp. You wisely, obtain some sweeties to sooth the neonate and warmed gel for ease of your bedside ultrasound exam.
A high-frequency linear transducer with copious amount of gel is now in your dominant hand with your non-dominant hand supporting the patient’s head. As you apply gentle pressure, the hyperechoic continuous cortical bone is immediately identified. You proceed to the affected side and find the left coronal suture, which is just anterior to the bruise.
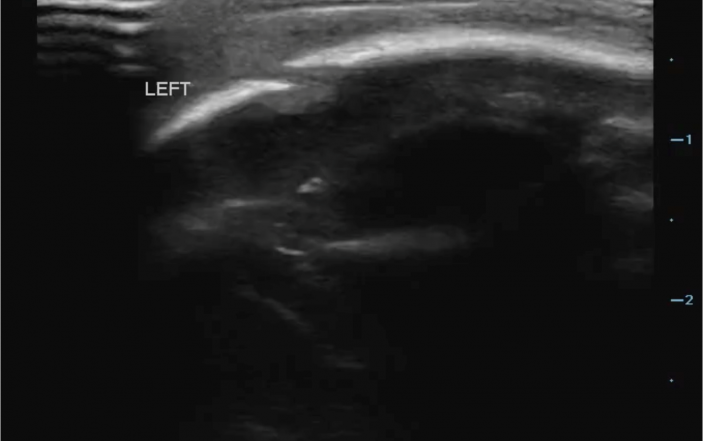
On the generated image, the linear hyperechoic scalp is now interrupted by hypoechoic cortical irregularity as you slide the transducer over the suture (Figure 1).

Depiction of skull fracture. Note cortical irregularity of the hyperechoic image.
To confirm the correct identification of the suture line and not the fracture, you trace the suture line to the anterior fontanelle (Figure 2). Using this as a reference point, you move transducer over the bruise and notice a similar finding, but conversely, the irregularity is not contiguous with any fontanelle. The exam is performed in two orthogonal planes, affirming your suspicion.

Cartoon representation of the neonatal skull with fracture.
A CT is immediately ordered after your bedside ultrasound finding (Figure 3).

Axial view of fracture on head computerized tomography (CT) of the skull.
You inform the parents of the ultrasound finding and place a consult to the neurosurgery team. As you patiently wait for the final impression, the patient is now NPO and is comfortably resting on her mother. The results of CT not only corroborates your bedside finding (Figure 2) with a developing subgaleal hematoma, but there is also a small subdural hematoma identified on the ipsilateral side. As a result, the patient is admitted to inpatient wards by the Neurosurgery team for observation.
Key Teaching Points:
- Incorporation of ultrasound into clinical practice should be done with great care and understanding of the limitations of the modality. Research into the topic has documented mixed results with sensitivity ranging from 77-100% and specificity ranging from 85-100%.(1-5)
- Many of the exams in the studies documenting ultrasound performance for skull fracture were performed by experienced sonographers, who are likely more experienced than the average practicing physician. As is the case with all ultrasound studies, results are dependent upon the skill of the sonographer.
- Ultrasound should not be utilized as a stand-alone test. The skill should be incorporated as part of the physical, history, and incorporation of a decision rule. PECARN gives clear indications for CT imaging; altered GCS, altered mental status, or signs of skull fracture on exam.(6) Additionally, CT should be strongly considered for patients younger than three months of age. If a patient does not fall within this realm, then CT versus observation is proposed based upon clinical factors. We feel that ultrasound can be best utilized in this observation versus CT imaging cohort. Identification of a skull fracture is associated with a higher likelihood of intracranial process.(5) Further risk stratification based upon ultrasound results in this observational cohort provides more information than history and physical alone.
- When performing this exam, select the highest frequency, linear transducer available. The higher frequency results in higher resolution and subsequent increased detail needed to evaluate for small cortical breaks.
- The area of focus is very superficial and reducing depth will help amplify the image on the screen. Bone on ultrasound should be bright, hyperechoic. Look for interruption of this hyperechoic boney cortex, which will represent fracture (Figure 1).
- Positioning the child in a position of comfort with the caretaker can help with exam cooperation. A cooperative patient is needed in order to thoroughly evaluate the area of interest. Utilize warm gel if possible and in areas of perceived pain use copious amounts to avoid direct pressure on a sensitive area. If available, consult your child life specialist to assist with the examination.
- When utilizing ultrasound to evaluate for skull fracture, the entire scalp does not need to be scanned. The research methods behind this topic focused scanning on the area of the hematoma or the area of impact.(1-5) Identified fractures are often found underlying a scalp hematoma. Scan the hematoma and the adjacent structures with fine detail. As is the case with most ultrasound applications, scanning in two planes will help increase accuracy.
Pearls and Pitfalls
- Skull fractures can be confused with suture lines. Knowledge of anatomy should be utilized when determining fracture versus suture. Use the symmetry of the skull to your advantage and scan the contralateral side if there is confusion. Findings of displacement, irregularity or jagged appearance on ultrasound often represent fracture.1,5 Sutures will be continuous with the fontanelle (Figure 2).
- Studies analyzing ultrasound identification of pediatric skull fracture have identified three areas where fractures have been missed: supraorbital region, lower occipital region, region adjacent to hematoma.1 Extra attention should be paid to these areas when the hematoma or area of impact includes these anatomic regions.
- It is important to note that patients without a hematoma can still have an occult skull fracture or intracranial injury, most noticeably those younger than three months of age as in the patient presented in this case.
References
- Choi, JY. Lim, YS. Jang, JH. et al. Accuracy of bedside ultrasound for the diagnosis of skull fracture in children aged 0-4 years. Pediatr Emer Care 2018; 00-00.
- Parri, N. Crosby, BJ. Glass, C. et al. Ability of emergency ultrasonography to detect pediatric skull fractures: a prospective, observational study. J of Emerg Med 2013; 44.
- Parri, N. Crosby, BJ. Mills, L. Point-of-care ultrasound for the diagnosis of skull fractures in children younger than two years of age. J Pediatr 2018; 196.
- Rabiner, JE. Friedman, LM. Khine, H. et al. Accurary of point-of-care ultrasound for diagnosis of skull fracture in children. Pediatrics 2013; 131(6).
- Riera, A. Chen, L. Ultrasound evaluation of skull fractures in children: a feasibility study. Pediatr Emer Care 2012; 28.
- Kuppermann, N. Holmes, JF. Dayan, PS. Identification of children as very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 2009; 374.



1 Comment
My wife thinks she has a crack in her skull.She was in a abusive relationship for over 10 years.I can feel something that feels like a crack in her skull.She has headache’s and she’s Real sitsitive to light.
Is this possible?