The term “Standard of Care” has been misused and abused. It is time to replace it with a phrase which more accurately conveys the realities of modern medicine.
The term “standard” has become ubiquitous in our everyday conversation. In some cases, the term is used appropriately. For example, it is standard treatment to give antibiotics for bacterial pneumonia, and it is standard management to provide PCI or thrombolytics for a STEMI. However, the more that we look at syntax and semantics, the more we realize that the term “standard” isn’t quite … well … standardized. Standard socket sets all have the same sizes, but standards of living vary dramatically between countries. Even in what we consider “standard” treatment for pneumonia, there is considerable variance. Should patients with bacterial pneumonia receive ceftriaxone, levofloxacin, piperacillin/tazobactam, azithromycin, vancomycin, another antibiotic or a combination of antibiotics? The answer can’t be defined by a single “standard” but instead becomes an inquiry as to what is a reasonable practice under the specific circumstances. Perhaps a healthy patient with a community-acquired pneumonia might only need azithromycin, a child would benefit from high-dose amoxicillin, a patient with multiple co-morbidities would require hospitalization and multidrug treatment and a patient with HIV might also need pentamadine and prednisone. In another variation on the theme, statisticians created the concept of a “standard deviation” realizing that samples in a data set may vary considerably.
Within the medical community, one phrase that is frequently misused is “standard of care.” It’s easy to allege that a practitioner failed to meet the “standard of care,” but in doing so, we have to consider the meaning behind those words. A standard is a “model” or “example” to be emulated. But there simply aren’t many “standards” in medicine. For example, there are many acceptable ways to manage hypertensive patients, to prescribe medications and even to physically examine patients. The problem with the notion of a “standard” is that it assumes everyone should be doing it all the time. That simply isn’t the case … legally or professionally.
Not only is the term “standard of care” often misused, it is often misunderstood. Consider a patient suffering from an acute ST elevation myocardial infarction. While the “standard of care” may dictate that the patient receives aspirin (even though, with a NNT of 42 [1], it is clear that not everyone benefits from this intervention), the same “standard of care” would dictate that the patient NOT receive aspirin if the patient was aspirin-allergic, the same “standard of care” would dictate that the patient SHOULD receive aspirin if the same “allergy” was merely GI upset, the same “standard of care” would be that the patient NOT be given aspirin if the patient already received aspirin in the ambulance on the way to the hospital, and there probably wouldn’t be a “standard of care” at all regarding whether the patient should receive aspirin in the hospital if he took aspirin with his other morning medications 6 hours prior to symptom onset. An expert who testified that there is a single “standard of care” regarding aspirin administration in acute myocardial infarction is either being untruthful or is incredibly naïve.
The legal definition of the “standard of care” is that which a reasonably competent and skilled physician would administer under the same or similar circumstances. Failing to meet the standard of care is simply another way of stating that a physician was negligent. However, it seems that many people don’t understand this nuance. In more than one deposition, I have seen experts testify that a physician acted “reasonably” but also violated the “standard of care” – as if these are mutually exclusive concepts. Another problem with the idea of a “standard” of care is that it may penalize innovators and early adopters who advance the knowledge of medicine. If a paper is published today that strongly supports a new intervention, and you order that intervention tomorrow, you’re providing reasonable medical practice and probably helping a patient, even though what you’re doing cannot yet be called “standard.”
Finally, medicine is as much an art as it is a science [2], focusing not only upon the medical pathophysiology but also upon each patient’s unique body, mind and soul. For this reason alone, each medical interaction is distinct, and there can be no “standard” that applies in every circumstance.
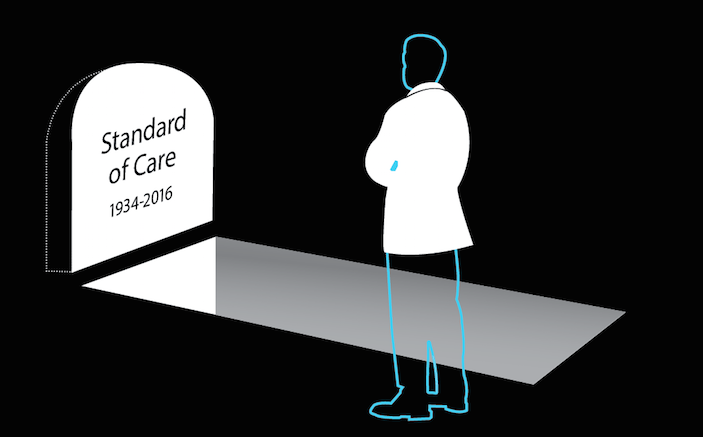
 When the meanings of words become prone to misunderstanding or misuse, they should be removed from our lexicon. It is time to retire the notion that there is some mythical “standard” of care to which every physician should adhere and be judged. The “standard” by which all human interactions are judged is one of “reasonableness,” and medical care should be no different. Reasonableness does not require perfection. Reasonableness only requires ordinary care and prudence.
When the meanings of words become prone to misunderstanding or misuse, they should be removed from our lexicon. It is time to retire the notion that there is some mythical “standard” of care to which every physician should adhere and be judged. The “standard” by which all human interactions are judged is one of “reasonableness,” and medical care should be no different. Reasonableness does not require perfection. Reasonableness only requires ordinary care and prudence.
For these reasons, we propose that the term “standard of care” be retired and replaced with “reasonable practice.” The terms are legally equivalent, but “reasonable practice” is far less prone to misinterpretation by experts and juries.
Beginning next month, we will be running a new column in EP Monthly by the same name: “Reasonable Practice.” We encourage you not only to adopt this new terminology for judging medical practice, but also to read the column to weigh in on whether the cases presented represent reasonable medical practices.
REFERENCES
- Lancet. 1988 Aug 13;2(8607):349-60. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. http://www.ncbi.nlm.nih.gov/pubmed/2899772
- Panda SC ‘Medicine: Science or Art? Mens Sana Monogr 2006 Jan-Dec; 4(1):127-138
http://www.msmonographs.org/article.asp?issn=0973-1229;year=2006;volume=4;issue=1;spage=127;epage=138;aulast=Panda



6 Comments
Thank you for this article – I agree wholeheartedly, the nomenclature has to change. As a provider who works in several different settings (inner city, academic, community, and international) there are definite variations to my practice and what would/ should be considered “reasonable” depending on where I’m working and the resources available there. Great piece!
Thank you, Dr. Sullivan, for bringing this to the fore. It’s better than keeping it as a burr under my saddle.
Parallel concepts: Standard of care medically: the dude in front, leading edge, top of class, 95%-er
Standard of care legally: the guy in the middle, 50%-er, ok for your family but not for mine.
Dr. Sullivan…
Your article and your very insightful analysis of the term “standard of care” is quite enlightening. I have always believed that anyone who attempted to codify a “standard of care” must be extremely naive or – shall I be the first to say it – an idiot.
However, as an attorney-friend once explained to me, the concept of “standard of care” really set the bar low, in the physician’s favor. I would hope that a changing of the term is not an attempt to set the bar even lower. While I cringe at the thought of an unfounded malpractice suit, I also cringe at the thought of some physicians practicing egregiously poor medicine but still covered by enough “reasonableness” to convince a jury that appropriate and reasonable care was indeed provided when, in fact, it was not. Within the last week I had the misfortune of observing an emergency physician (and I am myself a board-certified emergency physician) provide the poorest excuse for medical care that I have ever seen.
I do applaud you for pointing out that the term “standard of care” is basically useless, very prone to misuse and misunderstanding, and I certainly agree with tossing it from the medicolegal lexicon.
The legal term “standard of care” DOES, as Sullivan notes the legal definition, set the bar very low.
You may or may not agree with that precedent established by the judicial system over the years.
The problem, as Bill also notes, is that many “expert” witnesses have no IDEA what the legal definition of the standard of care is. see, e.g. “The Ethics of Being a Medical Expert Witness” http://www.ncbi.nlm.nih.gov/pubmed/16877139.
And this is never more true than when said (naive, idiotic, or simply dishonest and unethical) “expert” has been convinced by an attorney that “the standard” is something—anything— that did not happen in the current case. And that is why the use of the nebulous term “standard” should be abandoned.
“That degree of care which would be provided by a REASONABly competent physician practicing under the same or similar circumstances”, e.g. REASONABLE care, restates the legal definition much more accurately, would make much more sense to a jury; AND it would be much more difficult for a naive or willfully ignorant expert witness to misstate.
I do hope that Dr. Sullivan plans to publish this idea in legal publications as it is interesting but will of course never change the system if this idea is kept within the medical community.
I look forward to learning what we as a group consider REASONABLE care.
I have a very strong suspicion that it will be as diverse and difficult to define as was the STANDARD of care.
I agree that standard-of-care needs to go. It is highly subjective and is equivalent to passing a college course with a D-. I do not want D- care. Its replacement should be “evidence-based care.” This implies that the physician is fully knowledgeable about prevailing scientific evidence of how to diagnose and treat each patient. He should also know the limits of his knowledge and when to invite consultants to render an opinion. In my opinion, reasonable care is no better than standard of care from a patient’s point of view. I want best-evidence care.
The only time patients hear about “standards of care” is when they try to hold a hospital or physician accountable for harm. “The Hospital/doctor feels that the Standards of Care have been met” is almost always what these patients hear. It is also the standard comment when newspaper reporters contact them about a harmed patient they are writing about. What kind of an answer is that to someone who has suffered or even lost someone during a healthcare encounter? How about we create a a new measure of care , a new patient centered set of accepted standards created and used by patients with their doctors and hospitals. The Patients’ Expected Standard of Care, and have it only be about their outcomes, not the fancy services, pretty artwork, meals served, parking lot attendants and other amenities. It would be about the actual hands on medical and nursing care that led to either an excellent outcome or a preventable tragic outcome. As a retired ER nurse I know that not all tragic outcomes are preventable. And, I believe that most patients understand that too. Patients are the least recognized force and voice in healthcare today. Maybe it’s time to listen to them, their ideas and their very powerful stories, and to turn all of that into positive change. A simple change could be to always involve the patient or their advocate in any conversations about them, like a plan of care or a test, or a new medication, and after agreement, get their consent. Simple enough, but how often does it happen in an ER or any other hospital setting. Patients still basically get told what to do, like it or leave it. (or avoid it like I do!) I saw people get both lousy and delayed medical and nursing care in ERs, but I saw more miracles and that is why I worked in ERs for as long as I did. It was so amazing to be part of such meaningful work. I still believe that there are extremely dedicated and caring caregivers, but they need to find a way to partner up with their patients.