Introduction
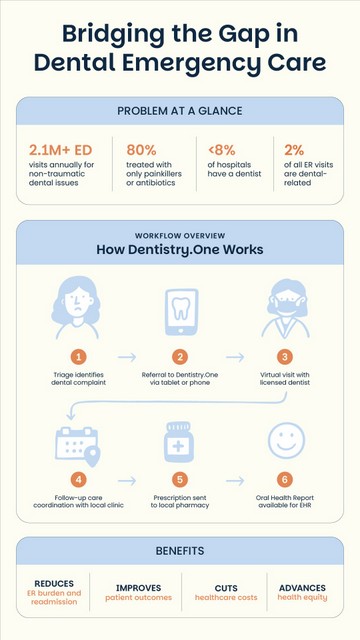
Each year, more than 2.1 million Americans turn to hospital emergency departments (EDs) for non-traumatic dental complaints such as toothaches, abscesses, or oral infections.¹
While these individuals often present in severe pain or distress, EDs are rarely equipped with the resources or personnel to resolve these conditions definitively.
In fact, more than 80% of dental-related ED visits result in the patient receiving only palliative care—typically in the form of analgesics or antibiotics—with no restorative treatment or long-term resolution.²
This disconnect between patient need and ED capability represents a critical inefficiency in the U.S. healthcare system. It also signals a missed opportunity for early intervention, continuity of care, and community-wide prevention.
The solution is access to a dentist at any time or from anywhere. This is accomplished via a scalable virtual-first dental care platform that can help hospitals, particularly those in rural and underserved areas, divert low-acuity dental emergencies from crowded EDs to qualified dental providers, improving outcomes while reducing costs.
The Hidden Burden of Dental Emergencies in the ED
Dental complaints account for an estimated $2 billion annually in emergency department expenditures.³ Nearly 95% of these visits result in discharge without admission, and often without resolving the source of the pain or infection.
This is because ED physicians typically lack dental training, and few hospitals have dentists on staff or the necessary clinical tools to perform extractions, restorations, or drainage procedures.2
According to the American Dental Association (ADA), fewer than 8% of U.S. hospitals employ a dentist or have an in-house dental clinic.⁵ This leaves emergency providers to manage oral pain using methods that do little more than delay definitive treatment.
What’s more, data from Oregon (2010) indicate that over 25% of patients with at least one ED visit for dental problems had multiple ED visits in the same year. About 21% had two to four visits in that year.
When it comes to kids aged 14 and under, recent CareQuest Institute Data states there was a significant increase in ED visits for non-traumatic dental conditions, rising from 27.3 to 43.1 visits per 10,000 people between 2019 and 2022.
For patients, the experience is frustrating. For hospitals, it’s resource-draining. For communities, it’s a missed opportunity to address oral health and its systemic health implications more comprehensively.
Disproportionate Impact in Rural and Underserved Settings
The burden of dental-related ED visits is even greater in rural areas, where access to routine dental care is limited. A 2018 ADA report found that rural EDs logged more than 80,000 visits for non-traumatic dental complaints in a single year.⁶ These comprised approximately 2% of all rural ED visits, a significantly higher proportion than in urban hospitals.
What’s more, rural residents are more likely to be uninsured or underinsured for dental services. They often live in designated dental health professional shortage areas (HPSAs), where the nearest provider may be hours away. In such regions, EDs serve as the default safety net for oral health crises; a role they are poorly suited to play.
Patients treated in the ED for dental pain frequently return weeks later with exacerbated symptoms. This cycle of inadequate care and repeat visits adds stress to an already strained rural health infrastructure.
The Clinical Limitations of the Emergency Department
Dental conditions commonly seen in the ED include toothaches, caries-related infections, cracked or avulsed teeth, and periodontal abscesses. While these conditions require specialized dental procedures, EDs are typically limited to offering temporary solutions.
One U.S. study reported that only 1.8% of all practicing dentists work in hospital settings.⁷ Even large urban hospitals may lack the equipment necessary for basic interventions like extractions. ED physicians are trained in acute medical care, not operative dentistry.
This results in a care model that stabilizes but does not resolve, palliates but does not prevent. Instead, patients are discharged with prescriptions, often opioids or antibiotics, and directed to find a dentist, a step that many, especially low-income or uninsured patients, never complete.
A Practical Alternative: Virtual-First Dental Triage
Virtual-first dental platforms utilizing teledentistry can close this gap. These platforms can serve emergency departments by providing real-time access to licensed dental professionals.
Using secure video consultations or asynchronous image reviews, a virtual-first dental platform can enable patients to receive timely evaluations and prescriptions while coordinating follow-up care with a local dental provider. Optimally, a platform with a network of care advisors can help ensure that patients are not only treated for acute symptoms but guided into a localized continuum of dental care. By diverting patients before admission to the ED, and then supporting care navigation, patient experiences and outcomes improve while saving costs and time.
Workflow Integration: How Virtual Dental Triage Operates in the ED
The integration process is straightforward and can be tailored to hospital protocols:
- Triage and Identification: Upon arrival, the triage nurse or admitting provider identifies a patient with a non-traumatic dental complaint (e.g., toothache, swelling, abscess).
- Virtual Referral: Instead of launching a conventional ED workup, the provider refers the patient to a virtual dental care partner using a QR code or URL via a hospital-supplied tablet or the patient’s own smartphone.
- Teleconsultation: A licensed dentist remotely evaluates the case via synchronous video or asynchronous photo review. They assess urgency, recommend a care plan, and issue prescriptions when appropriate.
- Care Coordination: If in-person care is required, a virtual care advisors can schedule a visit with a local dental practice or community clinic. Transportation or case management support may also be arranged.
- Documentation and Handoff: A full clinical report is generated and shared among dental and medical providers. This ensures continuity for providers and accountability in follow-up.
In some cases, this process can be initiated in under 10 minutes and enables hospitals to redirect patients quickly and responsibly without sacrificing quality or safety.
For example, Arrow Dental, a Medicaid-serving dental group in Oregon, integrated virtual dental care services to address after-hours emergencies and divert unnecessary ER visits.
Since implementation, the group has reported measurable reductions in ED utilization and improved patient access to timely care. The result is better continuity of care, improved clinical outcomes, and greater patient satisfaction.
System-Level Benefits for Hospitals and Communities
Integrating virtual dental care into ED workflows can yield several system-wide benefits:
- Reduces unnecessary ED use: Redirects low-acuity dental complaints, freeing up ED beds and reducing crowding.
- Lowers costs: Virtual consultations cost a fraction of in-person ED care.
- Improves quality and satisfaction: Patients receive diagnosis and treatment guidance from a licensed dentist rather than temporary relief.
- Facilitates continuity of care: Patients are not lost to follow-up but actively guided to the next step in their treatment.
- Promotes equity: Especially in rural and underserved settings, Dentistry.One can help fill persistent gaps in access.
Policy Trends and Telehealth Momentum
The COVID-19 pandemic accelerated the adoption of telehealth across all disciplines. Dentistry is no exception. State and federal regulations have expanded coverage for teledentistry, and payers are increasingly recognizing its cost-effectiveness for triage and urgent care.
A 2024 scoping review published in BMC Emergency Medicine found that non-ED interventions, including virtual triage, are effective at reducing low-acuity visits and improving resource allocation.⁸ These findings support further investment in virtual dental programs, particularly for institutions seeking to align with value-based care goals.
Conclusion
Emergency departments are indispensable for life-threatening medical conditions, but they are not designed for dental care. Redirecting non-traumatic dental complaints to virtual triage platforms like Dentistry.One is not only clinically appropriate, it’s economically and operationally smart.
Hospitals and health systems that integrate virtual-first dental solutions can reduce costs, relieve overcrowding, and deliver more appropriate care. At the same time, they serve their communities more effectively by connecting patients to the dental care they need and deserve.
References
- Agency for Healthcare Research and Quality. (2020). Emergency department visits involving dental conditions, 2018 (HCUP Statistical Brief #280). https://www.hcup-us.ahrq.gov.
- American Dental Association. (2019). Emergency department referrals. https://www.ada.org
- CareQuest Institute for Oral Health. (2020). Teledentistry: Providing access to care during the COVID-19 crisis. https://carequest.org.
- Cush, J., & Rodriguez, J. (2014). Reducing the use of hospital emergency departments for dental care. Dimensions of Dental Hygiene, 12(9), 36-40.
- Healthcare Cost and Utilization Project. (2020). Statistical brief #280: Most frequent reasons for emergency department visits, 2018. Agency for Healthcare Research and Quality. https://www.hcup-us.ahrq.gov
- Cohen, L. A., Manski, R. J., & Magder, L. (2016). Expanding the physician’s role in addressing the oral health of adults. American Journal of Public Health, 106(8), 1359–1361. https://doi.org/10.2105/AJPH.2016.303299
- Jacobsen, J. T., et al. (2024). Non-emergency department (ED) interventions to reduce ED utilization: a scoping review. BMC Emergency Medicine, 24, Article 28. https://doi.org/10.1186/s12873-024-01028-4
Photo Credit: Adobe