“Seeing is believing” you mutter as you shake your head in amazement. You can’t believe your good luck tonight. You ordered a CT scan on a patient with pleuritic right-sided chest pain looking for a pulmonary embolism, and instead you found her leaking thoracic aortic aneurysm. And then, your senior resident performed a bedside abdominal ultrasound on a 40-year-old male with chronic back pain and discovered a 5 cm abdominal aortic aneurysm.
“I can’t believe the pathology we see here!” your spunky new intern exclaims. “Lucky for him, but too bad for us, this new guy in the trauma bay isn’t going to have anything cool.” In the midst of all of the “cool cases” you’ve seen tonight, you are inclined to agree with your intern that the next one in the queue might just be a run-of-the-mill Friday night bar brawl gone bad. He’s a 40 year old who looks like he could probably use a self-defense class and a week or so in rehab. In between mumbling about his wallet and his iPhone, the guy doesn’t seem to be complaining about much. Your intern has completed a pretty comprehensive primary and secondary survey, and the only thing she’s found is extensive, bilateral periorbital edema and some suspected facial fractures by exam.
You ask her what the patient’s ocular exam showed, and she says she was just about to go back and take a better look with the senior resident. With all of the edema and ecchymosis, she couldn’t get a good look at the patient’s eyes without assistance. You walk her through some tips and tricks on how to pry open the swollen lids, and give her a list of things she needs to rule-out on exam.
After you help the rest of your team discharge a few more patients, you walk up to the trauma bay and beam with pride as your new intern and one of your senior residents is performing a bedside ocular ultrasound on Mr. Bar Brawl. With all of the edema on exam, they have decided it would be prudent to do a screening B-mode scan before they put the patient at risk for any more orbital or ocular trauma.
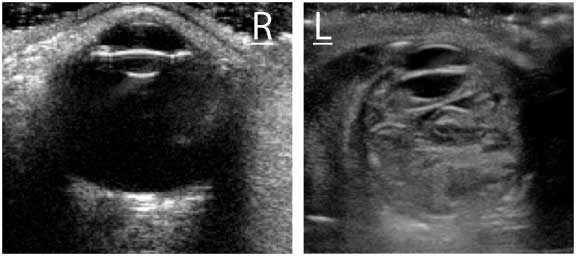
To avoid worsening any pre-existing injury, they float the linear array transducer lightly over his left eye and obtain the image above (right).
Satisfied with their view of the left eye, they slide the transducer over the right eye and do the same, obtaining this image (left).
click on image to enlarge

What abnormalities do you note on ocular ultrasound?
Conclusion in the following
Dx: Globe Rupture on Ultrasound
The right eye appears normal on ultrasound. The anterior chamber (AC), lens, and vitreous body appear atraumatic on the scan (above).
In contrast, the left eye appears grossly abnormal and you suspect your intern has picked up one of the most interesting cases of the night. The lens appears grossly intact, but the anterior chamber is flattened, and the vitreous body is filled with hyperechoic contents, likely clotted blood, mixed in with the vitreous humor. (below).
 You suspect that the patient has sustained a globe rupture from blunt orbital trauma and your team moves quickly to notify ophthalmology and plastic surgery of their new patient. As your battered and bruised bar-brawling patient gets wheeled off to the CT scanner to evaluate for other associated injuries, your intern gives you a thumbs up sign and remarks, “Now THAT was totally cool! Seeing really IS believing.”
You suspect that the patient has sustained a globe rupture from blunt orbital trauma and your team moves quickly to notify ophthalmology and plastic surgery of their new patient. As your battered and bruised bar-brawling patient gets wheeled off to the CT scanner to evaluate for other associated injuries, your intern gives you a thumbs up sign and remarks, “Now THAT was totally cool! Seeing really IS believing.”
Pearls & Pitfalls for Diagnosing a Globe Rupture on Bedside US
1. Globe ruptures are true ophthalmologic emergencies and often times, the diagnosis can be difficult to make based on exam findings alone.
2. The physical exam is often hindered by orbital edema or limited by patient discomfort and poor cooperation.
3. In blunt trauma, the ruptures are most common where the intraocular muscles insert on the sclera. The globe becomes thinner at those junctures and traction from blunt mechanisms can lead to small tears.
4. When you suspect that your patient has a globe rupture, care must be taken to minimize the amount of pressure placed on the globe. Direct pressure on the orbit can cause further extrusion of intraocular contents.
5. Bedside ultrasound, if used with care, can aid in rapid diagnosis of ocular conditions without causing harm.
6. Use the high frequency linear array transducer (7-10 MHz).
7. Apply a copious amount of water-soluble gel over the patient’s eyelid or use an acoustic stand off pad to enhance visualization of the globe and intraocular contents.
8. Float the probe in a transverse fashion over the gel. Take special care to ensure that pressure is not placed on the closed eyelid. Also avoid scanning the eye continuously for more than 60 seconds at a time.
9. Attempt to visualize the anterior chamber, the lens, the posterior chamber/vitreous body, the retina, the circular borders of the orbit, and the retrobulbar space.
10. Findings of a globe rupture include a flattened anterior chamber, abnormal lens positioning or lie, scleral buckling, an irregularly shaped or flattened vitreous body, or evidence of blood filling the posterior chamber mixed with vitreous humor.
11. Bedside ultrasound findings should be correlated with the physical exam and computed tomography findings if the diagnosis is uncertain.
12. The normal, contralateral eye can be used for comparison when subtle sonographic findings are in question.
13. Practice! Practice! Practice! With bedside ultrasound, there is no substitute for experience. The more scans you do, the better you will be able to differentiate abnormal from normal, even when you may not be sure exactly what the abnormality is.
An image library of normal and abnormal ultrasounds helps immensely, and we can help. Go to ERPocketBooks.com.