A 28-year-old female presented to the emergency department complaining of right-sided neck pain and swelling for the past 10 days.
In addition, she stated she had neck stiffness, trismus, odynophagia, headache, difficulty breathing, right-sided chest pain and fever of 104.0 F measured at home. She had taken five days of a friend’s amoxicillin and trimethoprim-sulfamethoxazole without improvement.
Her past medical history was significant for current intravenous drug use, untreated hepatitis C and multiple abscesses.
In the emergency department, she appeared in moderate distress with vital signs of blood pressure of 126/82, heart rate of 113 bpm, temperature of 99.0 F, respirations of 16 rpm and oxygen saturation of 96% on room air.
Physical exam demonstrated swelling to the right neck extending inferiorly from the right ear down to the right clavicle involving the right submandibular space with overlying erythema and a sub-centimeter area of spontaneous serosanguinous drainage over the right lower anterior neck (figures 1-2). No crepitus or meningeal signs were present. The patient did not exhibit any respiratory distress or stridor.
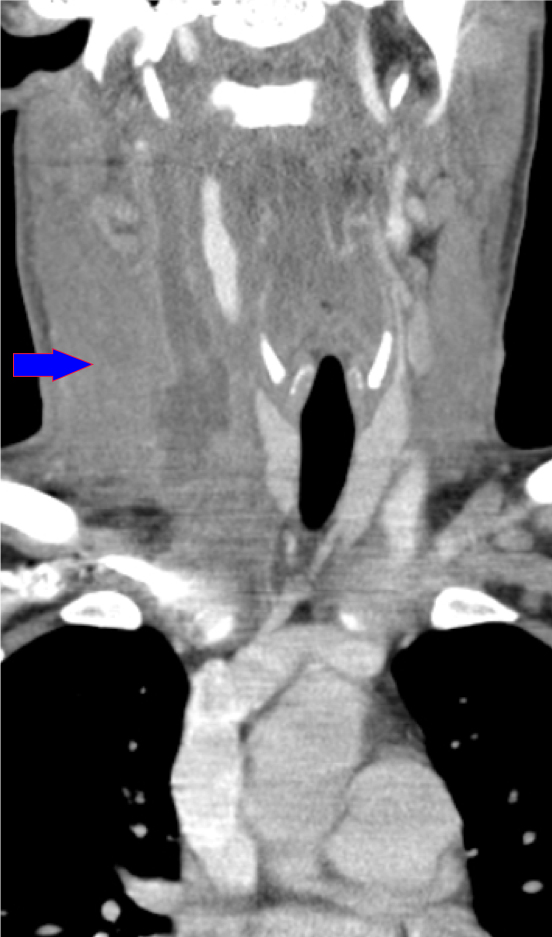
Laboratory evaluation was significant for a leukocytosis of 13.6 k/uL, CRP of 25.6 mg/dL, ESR of 107 mm/Hr, lactate 1.7 mmol/L and an anion gap of 16. A CTA of the neck with IV contrast was obtained and demonstrated severe thrombophlebitis of the right internal jugular vein with expansion of the vein with thrombus and purulent material extending from the skull base down to its confluence of the subclavian vein and evidence of leakage of purulent material outside the wall of the jugular vein.
Additionally, it showed extensive pyomyositis of the right sternocleidomastoid muscle with edema extending into the oral pharyngeal and hypopharyngeal walls with mass effect on the area and retropharyngeal edema (figures 3-6).
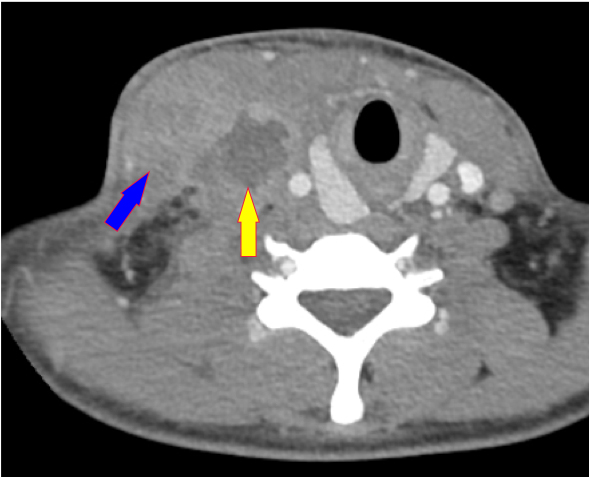
Figure 3: yellow arrow: thrombosed right IVJ with central area of hypodensity due to thrombosed IVJ; blue arrow: swollen and edematous sternocleidomastoid (SCM) muscle due to infective and inflammatory changes
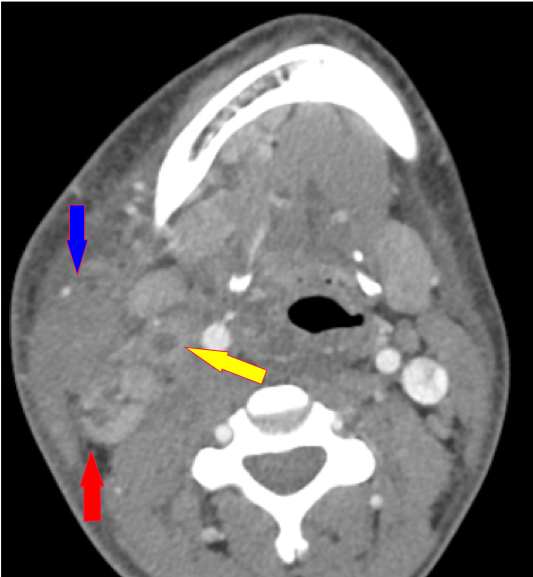
Figure 4: red arrow: enlarged lymph node; note fat stranding on the right side of the neck due to inflammatory changes; yellow arrow: thrombosed right IVJ; blue arrow: swollen and edematous SMC muscle
Per the radiologist, a nonspecific nodular density in the right middle lobe was noted and septic emboli could not be excluded.
The patient received vancomycin and piperacillin-tazobactam in the emergency department and she was admitted to the hospital for continued antibiotics. Blood cultures were eventually negative and wound cultures grew Group A streptococcus and staphylococcus aureus.
She was evaluated by infectious disease who recommended continued vancomycin and switching to ampicillin-sulbactam. Vascular surgery was consulted who recommended anticoagulation according to CHEST guidelines and continuation of antibiotics as treatment for septic thrombophlebitis.
Otolaryngology was consulted who performed incision and drainage of her neck with nasopharyngoscopy demonstrating widely patent airway. They recommended considering anticoagulation for a clinical picture likely representing Lemierre’s-like syndrome. The patient received two days of IV antibiotics and anticoagulation with heparin followed by enoxaparin with clinical improvement. She ultimately elected to leave the hospital against medical advice and was lost to follow-up.
Lemierre’s syndrome is a rare complication of bacterial pharyngitis or tonsillitis which typically involves an extension of the infection into the lateral pharyngeal spaces of the neck and resultant septic thrombophlebitis of the internal jugular veins (1). This condition was highlighted initially in 1936 by Andre Lemierre after he published a case series of 20 patients with a clinical syndrome of recent oropharyngeal infection, evidence of internal jugular thrombosis and anaerobic bacteremia primarily caused by Fusobacterium necrophorum (1,4). He described this syndrome as “anaerobic postanginal sepsis.”
After the year 1980, this condition was more routinely referred to as Lemierre’s syndrome(2). The worldwide incidence of Lemierre’s syndrome is estimated to be 1 in 1,000,000 and typically affects young, otherwise healthy patients. Approximately 90% of the patients diagnosed with Lemierre’s syndrome fall between the ages of 10 and 35 years old (1,2).
The commonly accepted pathophysiology of Lemierre’s syndrome is a precipitating bacterial or viral oropharyngeal infection leading to local mucosal damage and swelling, followed by lateral extension of the infection to the soft tissues of the neck (3).
This creates venous compression, stasis and ultimately a hypercoagulable environment. Venous thrombosis is initially within the peritonsillar veins but extends laterally and distally into the internal jugular veins (1).
Lemierre’s-like syndrome, attributable to intravenous drug use, has been reported in the literature though with less frequency (5). In this patient’s case, the infection was presumed to be a result of direct introduction by way of intravenous injection.
Diagnosis hinges on the use of CT imaging of the neck and chest with contrast, wound and blood culture data in combination with clinical features (6). Ultrasonography of the neck can be used as an alternative modality for detecting internal jugular vein thrombosis, however it is less sensitive than CT and cannot adequately visualize regions deep to the mandible or clavicle (6).
Treatment of Lemierre’s syndrome as well as Lemierre’s-like syndrome focuses on source control with drainage of abscesses when possible and IV antibiotics. Antibiotic coverage should be directed toward anaerobes such as Fusobacterium necrophorum, streptococcal species and bacteroides. This usually consists of piperacillin-tazobactam, ambicillin-sulbactam or carbapenems for at least 3-4 week (4,6).
In the setting of intravenous drug use, vancomycin should be considered for coverage of staphylococcal and streptococcal species. There is currently no definitive recommendation for or against anticoagulation as treatment for septic thrombophlebitis and the decision to anticoagulate should be based on the individual clinical scenario(7).
The estimated mortality rate of Lemierre’s syndrome in the modern, post-antibiotic era is 0-18% depending on the study (8,9).
Complications associated with Lemierre’s syndrome include disseminated intravascular coagulation, propagation of thrombosis superiorly into the intracranial sinuses or inferiorly into the subclavian vein, meningitis and septic embolic lesions (8,9).
References
1. Allen BW, Anjum F, Bentley TP. Lemierre Syndrome. [Updated 2023 Jul 31].
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023
Jan.
2. Eilbert, W., Singla, N. Lemierre’s syndrome. Int J Emerg Med 6, 40 (2013).
https://doi.org/10.1186/1865-1380-6-40
3. Wright WF, Shiner CN, Ribes JA: Lemierre syndrome. South Med J
2012,105(5):283-288. 10.1097/SMJ.0b013e31825581ef
4. Kuppalli K, Livorsi D, Talati NJ, Osborn M. Lemierre’s syndrome due to
Fusobacterium necrophorum. Lancet Infect Dis. 2012 Oct;12(10):808-15.
doi: 10.1016/S1473-3099(12)70089-0. Epub 2012 May 25. PMID: 22633566.
5. Galyfos G, Palogos K, Kavouras N. Septic internal jugular vein thrombosis
caused by Fusobacterium necrophorum and mediated by a broken needle.
Scand J Infect Dis. 2014 Dec;46(12):911-5. doi:
10.3109/00365548.2014.952247. Epub 2014 Oct 7. PMID:25290582.
6. Golpe R, Marin B, Alonso M. Lemierre’s syndrome (necrobacillosis).
Postgrad Med J. 1999 Mar;75(881):141-4. doi: 10.1136/pgmj.75.881.141.
PMID: 10448489; PMCID: PMC1741175.
7. Hoehn KS. Lemierre’s syndrome: the controversy of anticoagulation.
Pediatrics. 2005 May;115(5):1415-6. doi: 10.1542/peds.2005-0138. PMID:
15867055.
8. Leugers CM, Clover R: Lemierre syndrome: postanginal sepsis. J Am Board
Fam Pract 1995, 8(5):384-391.
9. Sinave CP, Hardy GJ, Fardy PW: The Lemierre syndrome: thrombophlebitis
of the internal jugular vein secondary to oropharyngeal infection.






1 Comment
Was this related to xylazine use?