You may think you know everything about the humble pee test, but there are subtleties you might be missing.
A 53-year-old female presents with malodorous urine. She denies dysuria, urgency, incontinence, and frequency, but she is concerned for UTI. She had one UTI several years ago, but at that time had dysuria and urgency. A urinalysis sent from triage demonstrates 3 WBCs, trace LE, and 2 squamous cells, but nitrites are negative. A diagnosis of UTI is made. Is this the right call?
URINALYSIS/URINE DIPSTICK AND ITS COMPONENTS
Urinalysis and urine dipstick are commonly ordered tests in the ED and can be useful in many clinical conditions, including urolithiasis and urinary tract infection (UTI). [1-5] Where can we go wrong? You may think you know how to interpret these tests, but there are several subtleties. In this article we’ll evaluate several components, including bedside analysis, dipstick, and pitfalls in analysis (especially in UTI).
METHOD OF COLLECTION
The most common collection method is midstream cleancatch into a clean dry container, while others include urethral catheterization or suprapubic aspiration. [2,3,6,7] Though external cleaning is usually recommended for midstream collection, it really does not have proven benefit in decreasing contamination. [1,3] One study found contamination rates were similar between those with and without cleansing. [6]
Even with external cleansing, close to 30% of samples are contaminated. [6] Once urine is collected, it should be rapidly analyzed, as bacteria can proliferate in warm urine. If the sample cannot be analyzed quickly, refrigeration is recommended. A delay of two hours or more can produce unreliable results. [3]
BEDSIDE ANALYSIS
First, let’s make one thing clear: only obtain urinalysis/urine dipstick if it will assist your decision making. Do not order it on a routine basis. Second, urine dipstick is comparable to microscopic analysis, with similar sensitivity and specificity. [8-10] Urine is normally a shade of yellow that darkens with greater pH or higher concentration. Medications, foods, metabolic conditions, trauma, and infection can change urine color (e.g., Pseudomonal infection resulting in a green appearance of urine or white urine with phosphate crystals). [3,4] Normal urine is transparent. Cloudy urine may be due to red blood cells, epithelial cells, bacteria, deposits, and crystals. Mucous, sperm, skin cells, normal urine crystals, and even body lotion/powders can result in more opaque urine. Urine odor can also be sweet (DKA resulting in acidosis and ketosis), ammonia-like (retention, urine standing at room temperature), musty (tyrosinemia), or several others. Fecal odor suggests GI fistula. [3,4,11]
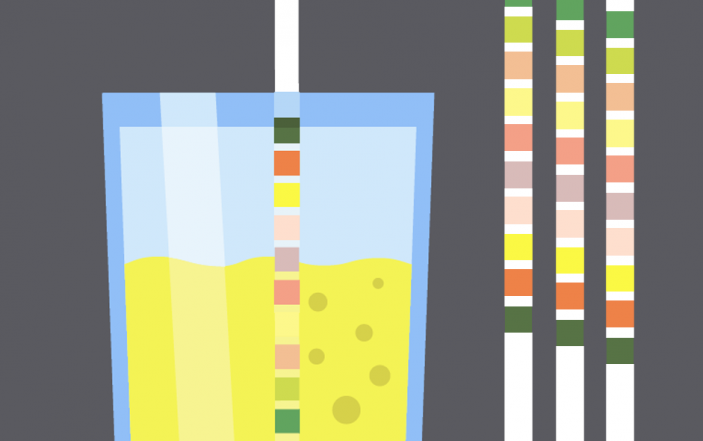
DIPSTICK ANALYSIS
Urine dipstick is a rapid semiquantitative series of tests on a reagent strip. Though often considered reliable, false positive and false negative results may occur. Testing with outdated or improperly stored dipstick material can inappropriately affect results. Components of dipstick include specific gravity, pH, protein, leukocytes, nitrites, blood, ketones, glucose, bilirubin, urobilinogen, bacteria, and squamous cells. [3,4,11]
Specific gravity is related to serum and urine osmolality, measuring the kidney’s ability to concentrate or dilute urine. Normal values range from 1.003 to 1.030 (< 1.010 is associated with relative hydration, while > 1.020 is associated with relative dehydration). [3,4,12] Decreased values occur with excessive hydration, nephrogenic diabetes insipidus, glomerulonephritis, pyelonephritis, and acute tubular necrosis.
Increased levels are found in dehydration, SIADH, adrenal insufficiency, liver failure, nephrotic syndrome, and prerenal renal disease. [3,12] It can also occur with glycosuria, proteinuria, IV contrast, and urine contamination.
Fixed levels approaching 1.010 are common in end stage renal disease or chronic glomerulonephritis. Urinary pH in patients with normal metabolic activity ranges from 5.5-6.5 (though some regard 4.5-8 as normal). [3,4] High urinary pH is common in vegetarians, UTIs (due to urea-splitting bacteria), alkalemia, type 1 renal tubular acidosis, and drugs. Lower urinary pH is common in diets with high protein or fruit, acidemia (the normal renal response to acidosis is acid excretion in the urine), diabetes, starvation, diarrhea, and several metabolic disorders (Phenylketonuria). [13-15]
Protein is often excreted in the urine, though this should not be greater than 150 mg in 24 hours. Levels of 150 mg/day are significant. Dipstick is positive for protein at 5-10 mg/dL. [3,13] However, microalbuminuria (30-300 mg/day) is usually not detected on dipstick testing. Results of 1+ correspond to 30 mg/dL, 2+ to 100 mg/dL, 3+ to 300 mg/dL, and 4+ to 1,000 mg/dL. [16,17]
Urine concentration can affect the semiquantitative results of the dipstick (dilute urine will result in underestimation of protein). A special indicator dye, Bromophenol blue, is most sensitive to albumin. However, it may not detect globulins and Bence-Jones proteins (secreted in multiple myeloma, lymphoma, and macroglobulinemia). [3,4,13] Urinary protein is elevated due to increased renal tubular secretion, increased filtration, pyelonephritis, glomerulonephritis, chronic hypertension, nephrotic and nephritic syndrome, drugs, CHF, exercise, fever, cold exposure, pregnancy, physiologic stress, and other conditions. [3,4,13]
Leukocyte esterase (LE) is an enzyme produced by neutrophils, and the presence of these cells is suggested with LE activity. A positive LE test is associated with pyuria, typically in the setting of > 10 WBCs per high powered field (hpf). [3,18,19] To properly evaluate for LE, the dipstick requires 30 seconds to 2 minutes of urine contact. There are many pitfalls with this test, which we will discuss later.
Nitrites are not normal in urine. These result from the conversion of urine nitrate to nitrite by bacteria, which typically requires approximately 4 hours of incubation within the bladder. [19,20] A positive nitrite test reflects the presence of gram-negative bacteria such as E. coli. A positive test is extremely specific, but not sensitive for UTI. [20,21]
Over 10,000 bacteria/mL urine is required to result in a positive nitrite test. Unfortunately, nitrite dipstick reagent strips are sensitive to air. After one week of exposure to air, up to 1/3 of strips provide a false positive result, which increases to 3/4 at two weeks. [22] Hematuria is defined by the presence of at least 3 RBCs/hpf on urinalysis. [3,4,23-25] Hemoglobin itself is typically poorly filtered, and the presence of hemoglobin in the urine occurs once haptoglobin is fully saturated and proximal reabsorption capacity is exceeded. On the other hand, myoglobin is smaller and not protein-bound. Urine dipsticks can also detect the presence of whole and lysed red blood cells through peroxidase activity.
Myoglobin and hemoglobin both catalyze this reaction (thus the positive test in rhabdomyolysis). A positive dipstick result may be due to trauma, infection, inflammation, calculi, neoplasm, clotting disorder, burns, cold, eclampsia, sick cell crisis, transfusion reaction, exercise, and infarction. Diets with high vitamin C can result in false negative results for hematuria, as vitamin C affects peroxidase activity. [3,4]
Glucose is typically filtered in the glomerulus and reabsorbed in the proximal tubule. However, glycosuria can occur when the filtered glucose exceeds the tubules ability to reabsorb (serum levels 180-200 mg/dL), seen in diabetes, Cushing’s disease, liver disease, and several congenital/metabolic conditions. [3,4] Another cause is failure to resorb urinary glucose in the proximal tubule.
Ketones result from incomplete fat metabolism, accumulate in the serum, and are then excreted in the urine. Low carbohydrate diets, starvation, diabetes, alcoholism, hyperthyroidism, and eclampsia can result in increased urinary ketones. Other causes include insulin, isoniazid, and isopropyl alcohol overdose. Most labs use the nitroprusside test for detection of ketones, which is more sensitive to acetoacetic acid, rather than beta-hydroxybutyric acid (the predominant ketone in DKA). [3]
Bilirubin is not normally found in urine. Unconjugated bilirubin is not filtered, as it is not water soluble; however, conjugated bilirubin is water soluble. Its presence in urine is suggestive of liver or biliary dysfunction. Urobilinogen is present in small amounts in urine. This is the end product of bilirubin metabolism. Hemolysis and liver disease can increase urine urobilinogen amounts, while bile duct obstruction and specific antibiotics may decrease it.
PITFALLS
With the basic background of urine, let’s start with the pitfalls. First, let’s examine the false positives and negatives (Table 1). [8,9,21,26-32] Later, we will evaluate dipstick and UTI specifically.

As demonstrated in Table 1, there are a significant number of false positives and negatives for urine dipstick, and the diagnosis of UTI is not always straightforward. [19] A diagnosis of UTI should not be based on dipstick or urinalysis alone. History and exam can be helpful in diagnosis of UTI. When UTI symptoms are combined with an absence of symptoms of vaginitis or cervicitis, the likelihood of UTI increases to over 90%, with positive likelihood ratio (LR) of 24! [33] Self-diagnosis of UTI has a positive LR of 4.[33] Let’s look at some pitfalls in dipstick analysis for UTI.
PITFALL #1: ASSUMING SQUAMOUS CELLS = CONTAMINATION
Classically, a “good” urine sample contains less than 5 squamous epithelial cells (SECs)/low-power field (lpf). [18,19] Recommendations have previously been to obtain a repeat sample for samples with > 5 SECs/lpf. However, SECs are poor markers of urine culture contamination. [33] One study evaluated a quantitative threshold of SECs. [33] In that study, samples with fewer than 8 SECs/lpf demonstrated greater ability to predict bacteriuria on urinalysis (+LR 4.98), but SECs did not accurately identify contaminated urine. [33]
Samples with the absence of pyuria and nitrites perform similarly no matter the SEC count in the specimen. For culture, no threshold of SECs predicts contamination. [33]
PITFALL #2: ASSUMING CLOUDY, SMELLY URINE = UTI
Unfortunately, urine color, clarity, and odor cannot be used to diagnose UTI.19 One study found a 13% sensitivity for urine transparency to diagnose UTI. [35] As discussed, cloudy urine has a variety of causes and is common with crystals and purine-rich food. Foul-smelling odor cannot be used in spontaneously voiding or catheterized patients to diagnose UTI, and urine odor is primarily dependent on the patient’s urea concentration in the urine and hydration status. [36,37]
PITFALL #3: CONCLUDING POSITIVE LE AND/OR WBC = UTI
Urinalysis with positive LE alone should not be used for diagnosis of UTI. [19] Positive LE demonstrates sensitivity 80-90% and specificity 95-98% for pyuria. [8,18,33] WBC counts of 6-10 cells/mL may be due to dehydration, and patients with oliguria or anuria also commonly have pyuria. [3,8,19] Many conditions can result in sterile pyuria, including contamination, interstitial nephritis, nephrolithiasis, tumor, interstitial cystitis, intraabdominal pathology, and presence of an atypical organism.
Overtreatment occurs in up to 44% of patients if WBC count alone is used with cutoff of 3 WBC/hpf. [8] True symptomatic UTI is associated with a significant number of WBCs in the urine (> 10/microL). [19] Hematuria can cause a false positive result for urine WBCs. Leukocytes and WBCs may be present in urine due to other conditions such as appendicitis, diverticulitis, sexually transmitted infection, and renal injury. False negatives can occur in neutropenic/leukopenic patients. [3,4] Rather than relying on UA alone, diagnosis should be based on patient symptoms.
PITFALL #4: CONCLUDING POSITIVE NITRITES = UTI
Positive urinalysis for nitrites possesses high specificity for gram-negative bacteriuria. [3,4] However, urine nitrites in isolation are not diagnostic of UTI. [19] Symptoms of UTI in association with positive nitrite are diagnostic of UTI. On the other hand, nitrite testing may be negative with insufficient urine dwell time in the bladder or infection with organisms unable to convert nitrate to nitrite. [3,4] In this setting, other components of the dipstick should be used in conjunction with symptoms of UTI for diagnosis.
Negative LE and nitrite can rule out UTI in uncomplicated and complicated patients with a sensitivity approaching 94%, and a patient with urinary symptoms and negative LE and nitrite should undergo evaluation for other causes of symptoms. [38] Positive LE and nitrite together display a sensitivity for bacteriuria of 48% and specificity of 93% in nursing home patients. [39] Specificity approaches 100% in other populations. [9]
BONUS ROUND: URINE PREGNANCY TESTING
Pregnancy testing can be completed on serum or urine samples. Urine testing is typically qualitative, though this is less sensitive than serum testing (which can be quantitative or quantitative). [40,41] While serum pregnancy tests can detect hCG levels of 5-10 milli-int. units/mL, and high sensitive quantitative serum tests are positive at 1-2 milli-int. units/mL, urine qualitative tests are not far behind, with positive results at 20-50 milli-int. units/mL – and these assessments are accurate and reliable with current assays. [40-42]
Importantly, other urine factors such as specific gravity have not been shown to affect qualitative urine testing for pregnancy, even with specimens diluted fivefold. [42-44] False negatives can occur in the setting of early pregnancy in which the hCG is below the threshold of detection, or a hook effect, where a very high hCG is present and affects test reagents. [42,45]
BOTTOM LINE
Labs should only be used to supplement, not replace, clinical decision making. If the patient has symptoms consistent with UTI, order urinalysis and treat with antibiotics if positive. If the non-pregnant patient does not have symptoms consistent with UTI but urinalysis is positive for LE, nitrites, WBC, or bacteria, you should consider other conditions in concert with repeat testing and follow up.
CASE CONCLUSION
The patient denies all symptoms of UTI. She asks about the urine dipstick, and you tell her the results. You ask her about recent lifestyle changes, and she says she has had several steak dinners. She has also not been drinking her usual amount of water. You discuss the need for hydration and the risks of antibiotics. With absence of any UTI symptoms, you decide against antibiotics.
Stay tuned for Part II, where we will dive deeper into more complicated topics such as asymptomatic bacteriuria, ureteral stent, urinary diversion, and catheter-associated UTI.
REFERENCES
1. LaRocco MT, Franek J, Leibach EK, et al. Effectiveness of Preanalytic Practices on Contamination and Diagnostic Accuracy of Urine Cultures: a Laboratory Medicine Best Practices Systematic Review and Meta-analysis. Clin Microbiol Rev. 2016; 29:105.
2. Takhar SS and Moran GJ. Diagnosis and management of urinary tract infection in the emergency department and outpatient settings. Infect Dis Clin N Am 2014;28:33-48.
3.Simerville JA, Maxted WC, Pahira JJ. Urinalysis: A Comprehensive Review. Am Fam Physician. 2005 Mar 15;71(6):1153-1162.
4. Cadogan M. Urinalysis. LIFTL. https://lifeinthefastlane.com/investigations/urinalysis/. Accessed 10 December 2017.
5. Gupta K, Hooton TM, Naber KG, et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clinical Infectious Diseases. 2011; 52(5):e103 -e120.
6. Lifshitz E, Kramer L. Outpatient urine culture: does collection technique matter? Arch Intern Med. 2000;160:2537–40.
7. Hooton TM, Roberts PL, Cox, ME, et al. Voided Midstream Urine Culture and Acute Cystitis in Premenopausal Women. N Engl J Med. 2013 November 14;369(20):1883–1891.
8. Lammers RL, Gibson S, Kovacs D, et al. Comparison of test characteristics of urine dipstick and urinalysis at various test cutoff points. Ann Emerg Med. 2001;38(5):505-512.
9. Leman P. Validity of urinalysis and microscopy for detecting urinary tract infection in the emergency department. Eur J Emerg Med. 2002;9(2):141-147.
10. Walter FG, Knopp RK. Urine sampling in ambulatory women: midstream clean-catch versus catheterization. Ann Emerg Med. 1989;18(2):166-172.
11. Hanno PM, Wein AJ, Malkowicz SB. Clinical manual of urology. 3d ed. New York: McGraw-Hill, 2001.
12. Kavouras SA. Assessing hydration status. Curr Opin Clin Nutr Metab Care. 2002;5:519–24.
13. Sheets C, Lyman JL. Urinalysis. Emerg Med Clin North Am. 1986;4:263–80.
14. Kiel DP, Moskowitz MA. The urinalysis: a critical appraisal. Med Clin North Am. 1987;71:607–24.
15. Benejam R, Narayana AS. Urinalysis: the physician’s responsibility. Am Fam Physician. 1985;31:103 11.
16. House AA, Cattran DC. Nephrology: 2. Evaluation of asymptomatic hematuria and proteinuria in adult primary care. CMAJ. 2002;166:348–53.
17. Carroll MF, Temte JL. Proteinuria in adults: a diagnostic approach. Am Fam Physician. 2000;62:1333–40. 18. Pappas PG. Laboratory in the diagnosis and management of urinary tract infections. Med Clin North Am. 1991;75:313.
19. Schulz L, Hoffman RJ, Pothof J, et al. Top ten myths regarding the diagnosis and treatment of urinary tract infections. Journ Emerg Med. 2016;51(1):25-30. 20. Williams GJ, Macaskill P, Chan SF, et al. Absolute and relative accuracy of rapid urine tests for urinary tract infection in children: a meta-analysis. Lancet Infect Dis. 2010; 10:240.
21. Pels RJ, Bor DH, Woolhandler S, et al. Dipstick urinalysis screening of asymptomatic adults for urinary tract disorders. II. Bacteriuria. JAMA. 1989;262:1221–4.
22. Gallagher EJ, Schwartz E, Weinstein RS. Performance characteristics of urine dipsticks stored in open containers. Am J Emerg Med. 1990;8:121–3.
23. Mariani AJ, Mariani MC, Macchioni C, et al. The significance of adult hematuria: 1,000 hematuria evaluations including a risk-benefit and cost-effectiveness analysis. J Urol. 1989;141:350–5.
24. Grossfeld GD, Litwin MS, Wolf JS, et al. Evaluation of asymptomatic microscopic hematuria in adults: the American Urological Association best practice policy—part I: definition, detection, prevalence, and etiology. Urology. 2001;57:599–603.
25. Grossfeld GD, Litwin MS, Wolf JS Jr, et al. Evaluation of asymptomatic microscopic hematuria in adults: the American Urological Association best practice policy—part II: patient evaluation, cytology, voided markers, imaging, cystoscopy, nephrology evaluation, and follow-up. Urology. 2001;57:604–10.
26. Woolhandler S, Pels RJ, Bor DH, et al. Dipstick urinalysis screening of asymptomatic adults for urinary tract disorders. I. Hematuria and proteinuria. JAMA. 1989;262:1214–9.
27. Agarwal R, Panesar A, Lewis RR. Dipstick proteinuria: can it guide hypertension management? Am J Kidney Dis. 2002;39:1190–5.
28. Sultana RV, Zalstein S, Cameron P, Campbell D. Dipstick urinalysis and the accuracy of the clinical diagnosis of urinary tract infection. J Emerg Med. 2001;20:13–9.
29. Smith P, Morris A, Reller LB. Predicting urine culture results by dipstick testing and phase contrast microscopy. Pathology. 2003;35:161–5.
30. Van Nostrand JD, Junkins AD, Bartholdi RK. Poor predictive ability of urinalysis and microscopic examination to detect urinary tract infection. Am J Clin Pathol. 2000;113:709–13.
31. Eidelman Y, Raveh D, Yinnon AM, et al. Reagent strip diagnosis of UTI in a high-risk population. Am J Emerg Med. 2002;20:112–3.
32. Semeniuk H, Church D. Evaluation of the leukocyte esterase and nitrite urine dipstick screening tests for detection of bacteriuria in women with suspected uncomplicated urinary tract infections. J Clin Microbiol. 1999;37:3051–2.
33. Bent S, Nallamothu BK, Simel DL, et al. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002;287(20):2701–10.
34. Mohr NM, Harland KK, Crabb V, et al. Urinary Squamous Epithelial Cells Do Not Accurately Predict Urine Culture Contamination, but May Predict Urinalysis Performance in Predicting Bacteriuria. Acad Emerg Med. 2016;23:323–330.
35. Foley A, French L. Urine clarity inaccurate to rule out urinary tract infection in women. J Am Board Fam Med. 2011;24:474–5.
36. Nicolle LE. The chronic indwelling catheter and urinary infection in long-term-care facility residents. Infect Control Hosp Epidemiol. 2001;22:316–21.
37. Nicolle LE, Bradley S, Colgan R, et al. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:643–54.
38. Deville WL, Yzermans JC, van Duijn NP, et al. The urine dipstick test useful to rule out infections. A meta-analysis of the accuracy. BMC Urol. 2004;4:4.
39. Sundvall PD, Gunnarsson RK. Evaluation of dipstick analysis among elderly residents to detect bacteriuria: a cross-sectional study in 32 nursing homes. BMC Geriatr. 2009;9:32.
40. Davies S, Byrn F, Cole LA. Human chorionic gonadotropin testing for early pregnancy viability and complications. Clin Lab Med. 2003;23:257.
41. O’Connor RE, Bibro CM, Pegg PJ, Bouzoukis JK. The comparative sensitivity and specificity of serum and urine HCG determinations in the ED. Am J Emerg Med. 1993; 11:434.
42. Chard T. Pregnancy tests: a review. Hum Reprod. 1992;7:701.
43. Ikomi A, Matthews M, Kuan AM, Henson G. The effect of physiological urine dilution on pregnancy test results in complicated early pregnancies. Br J Obstet Gynaecol. 1998 Apr;105(4):462-5.
44. Neinstein L, Harvey F. Effect of low urine specific gravity on pregnancy testing. J Am Coll Health. 1998 Nov;47(3):138-9.
45. Griffey RT, Trent CJ, Bavolek RA, et al. “Hook-like effect” causes false-negative point-of-care urine pregnancy testing in emergency patients. J Emerg Med. 2013; 44:155.



5 Comments
High clinical relevance. We use this each shift.
Nice read.
As a urostomy patient, I am so grateful for the education you are providing on false negatives. I have suffered countless delays and even acute on chronic kidney failure because some docs wont listen re: false neg’s on urinalysis with reflex to culture. Urostomy pats do not have the necessary bladder cells to interact with the bacteria and turn nitratyes into nitrites. Add in a case of myelodysplasia and I also dont have enough wbc in my blood, much less my urine, to count as a sign for pos microscopic. Not sure what the luekocyte esterase issue is-but often get false negs on that too. Just had 2 false neg UA on a culture that wound up being greater than 100K klebsiella ESBL. Needless to mention: symptoms also different. Thanks for the 411
Good academic content
Hi, gentleman; I love your blog. It’s a great resource. I have a comment about Pitfall#1. It appears citation 18 is missing. I also looked at the JAMA article, which is a meta-analysis. Your post states, “One study evaluated quantitative thresholds…” I cannot find where this study mentioned SECs in the article. I’m wondering which study you are referencing. Thank you. Keep up the great work.