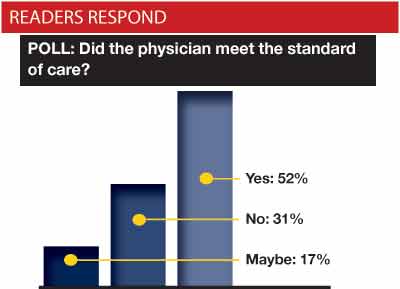
In the March issue, we asked EPM readers to weigh in on the scenario below, answering the question, “Did the physician meet the standard of care?” We received 186 detailed responses. William Sullivan, DO, JD offers a final case analysis.
THE CASE
A 72-year-old man with no prior medical history presents for evaluation of lower abdominal pain for the prior 24 hours. He has no history of fever, chills, or other symptoms. Vital signs are stable. On physical exam, the patient has minor lower abdominal pain but no guarding or rebound tenderness. Rectal examination shows mild prostatic tenderness on palpation. The remainder of the examination is normal. Lab tests showed a WBC count of 10.8 with no shift. Urinalysis had 5-10 WBCs but no bacteria. The patient was diagnosed with prostatitis and discharged with a prescription for ciprofloxacin.
While several responses to this scenario noted that more information needed to be provided in this case, the facts were taken from a jury verdict reporter which itself did not provide much information. The outcome of the case is at the end of this column.
In large part, this scenario essentially amounts to a description of what the standard of care should be when managing an elderly patient with acute abdominal pain. While I realize that there are multiple ways in which elderly patients can present with acute abdominal pain, I think it is important to consider some general literature regarding abdominal pain in elderly patients.
Elderly patients with abdominal pain are more likely to have serious medical problems that are not present in younger patients. Mesenteric ischemia and abdominal aortic aneurysms are uncommon in patients younger than 50 years old. The incidence of pancreatitis increases dramatically after age 65. Elderly patients also are more likely than younger patients to have gastrointestinal cancers, GI bleeding, diverticular disease, biliary disease, and intestinal volvuli.
In addition to an increased likelihood of serious medical problems related to their complaints of abdominal pain, elderly patients with abdominal pain are also more likely to have vague symptoms and nonspecific findings on their physical examination. Consider the following statistics regarding two causes of abdominal pain: Elderly patients with cholecystitis have no significant pain in 25% of cases, and less than half of elderly cholesystitis patients have a fever or elevated WBC count. Despite the vague findings, 10% of elderly patients diagnosed with cholecystitis will die from the disease. Similarly, elderly patients comprise only 5-10% of the cases of acute appendicitis, but account for 50% of the deaths from acute appendicitis. Only 20% of elderly appendicitis patients presented with classic appendicitis symptoms of anorexia, fever, right lower quadrant pain, and an elevated WBC count. Less than half of elderly patients with acute appendicitis had a temperature more than 99.7. Perforation of the appendix occurs in 4% of younger patients but occurs in 37% of elderly patients.
As a result of delayed presentation, nonspecific physical complaints, inconsistent physical findings, and increased risk of life-threatening diseases, elderly patients with abdominal pain are more likely to be misdiagnosed and are more likely to die from their conditions. Up to 40% of elderly abdominal pain patients are initially misdiagnosed, resulting in a mortality rate of 10%. Mortality rates in elderly patients with large bowel obstructions approaches 40% – often due to delays in diagnosis. Mortality rates in elderly patients suffering from pancreatitis is also close to 40%. Mesenteric ischemia has a 70-90% mortality rate. Despite widespread use of CT scans in the emergency department, studies have shown that 60% of elderly abdominal pain patients required hospital admission, 20% needed surgery, and 5% died.
During court testimony in this case, the defendant physician stated that he did not believe that the patient had appendicitis because the patient had no guarding or rebound on palpation. One study of geriatric inpatients (mean age of 82) with pathologically proven peritonitis showed that only 73% had abdominal tenderness and only 34% had guarding. While we obviously can’t generalize this study to all elderly patients, it does suggest that even pain is not a consistent finding in elderly patients with abdominal pathology.
The diagnosis of prostatitis in this case may have been plausible, but the patient lacked many of the typical findings of acute prostatitis – most notably any urinary symptoms such as frequency, urgency, dysuria, urinary hesitancy, or urinary retention. Mild prostatic tenderness as opposed to a hot, boggy, tender, inflamed prostate gland also argues against a diagnosis of acute bacterial prostatitis. However, choosing one plausible diagnosis over another diagnosis does not necessarily violate the standard of care.
When considering the nonspecific findings and the potential for serious medical conditions in elderly patients with abdominal pain, often further investigation of an elderly patient’s abdominal pain complaints is warranted. One study showed that 30-40% of elderly patients presenting to the emergency department with abdominal pain ultimately require surgical intervention. If 30-40% of patients with chest pain required open heart surgery, would any of us feel comfortable discharging chest pain patients with labs and a set of cardiac enzymes?
Because of the wide variance in history, presenting complaints, and physical examination, there isn’t a one size fits all algorithm that we can use for every elderly patient who has abdominal pain. Whether the standard of care was met in any specific case must therefore be determined on a case-by-case basis. Perhaps the only “take home” point from this case is that elderly abdominal pain patients are more likely to present with vague and nonspecific symptoms while harboring serious disease processes.
In this scenario, there is certainly room for debate as to what a reasonable physician would do under the circumstances presented (see graph of reader responses). However, given the increased potential for a serious medical problem coupled with fairly vague physical findings and with nonspecific laboratory tests, I believe that advanced imaging should have been performed prior to this patient’s disposition. A mandatory follow up examination in 12-24 hours to reassess his condition would also have been acceptable, but did not occur. Standard of care not met.
The epilogue to this case was that the patient returned 10 days later with worsening abdominal pain. A CT scan performed on the return visit showed that he had ruptured his appendix, cecum, and ileum. During surgery, the patient required a permanent ileostomy. He suffered a prolonged postoperative course in the ICU. The case settled for $350,000 before trial.
References:
- Tazkarji, MB, Abdominal Pain Among Older Adults: Differential Diagnosis. www.medscape.com. Accessed March 15, 2011.
- Bryan, ED. Abdominal Pain in Elderly Persons. www.emedicine.com. Accessed March 15, 2011.
- Burg, MD, Acute Abdominal Pain in the Elderly, Emergency Medicine, August 2005
- Marco CA, et al. Abdominal pain in geriatric patients: variables associated with adverse outcomes. Acad Emerg Med 1998
A Sampling of Reader Commentary
“In 30 years of EM practice, constipation and UTI have been misdiagnosed in the majority of patients who re-present with catastrophic causes of abdominal pains”
-Frank Parks
”We
need to get back to more clinical medicine when appropriate and not rely on expensive and often unnecessary tests just because we can do them.”
-Greg Amaya, MD
“It is acceptable to discharge a 72-year-old with abdominal pain, but only after a thorough history and physical exam.”
-Mark Goldstein
”In this case of an elderly man with mild pain and tenderness, who presumably does not have a pulsatile abdominal mass, abnormal pulses, etc… it is reasonable to conclude that the cause of the pain is prostatic inflammation.”
-William Jantsch, MD




4 Comments
Hard to prove that this patient had appendicitis when evaluated in the ED, but I agree with the writer in that abdo pain in elderly patient = badness until proven otherwise. We can also make a reasonable argument that after a complete H&P if nothing is found, it is safe to discharge an elderly patient with abdo pain. But the studies fail to support that approach in a significant way. The truth is that an older patient with abdo pain has worse mortality than that same patient with chest pain. Can’t argue against that. I think advanced imaging was needed and maybe prolonged obesrvation would have been more appropriate. But this is using the retroscope…
I agree.
My husband has pain in his lower right side and there’s a 72-year-old male with other underlying health conditions. He has no appendix. The pain has become debilitating and is escalating and he is currently in patient at the VA hospital in Little Rock. They were planning on discharging him after stating that all of his scans and labs were normal.
I immediately became involved and said that his pain has not been managed since 2017 and has now escalated to a point where I saw his gun lying on top of his neatly folded T-shirts in his dresser drawer – in all of our years of marriage this man has never so much as folded a handkerchief.
My response to the doctor’s husband that I want every single report in the name of every single doctor who treated him or touched him, who read a radiology report, performed a scan, etc. and that I would be taking my husband to either male clinic or to Loyola in Chicago where the northwest Arkansas good old boys doctors club that holds hands with the VA in Little Rock and UAMS will not interfere and continuously push my husband down an assembly line of “discharge with follow up to PCP”…..
I mentioned there is a liability someplace and I intend to find out who dropped the ball. I was informed that they would be getting second opinions for my husband‘s condition where he now waits for the eighth day at the VA hospital .
History taking in the elderly is sometimes difficult and prolonged, especially when there are other “critical” patients in the ED. This may have been a case of an early disease process at presentation, or maybe not. Regardless, I think this physician could have dodged a bullet by providing detailed discharge instructions with 24hr PCP follow up.
My mother has been living with extremely uncomfortable abdominal pain for the past five weeks. We who live in Fresno California are lucky for the Health care our Dr’s provide.We have not found any relief as of today;10/21/14……please help.
thank you.