Paramedics present to an urban emergency department with a middle aged man found unresponsive in a nearby alley. The paramedics were unable to obtain IV access due to years of drug abuse and overall poor venous access.
Physical Exam
- General: Middle aged male, unresponsive to painful stimuli
- Vital signs: P=57/min (sinus bradycardia) RR=5 breaths/min T=97.9 F
- BP: 165/90 mmHg Pulse Ox=98% on a non re-breather
- Head: normocephalic, atraumatic
- ENT: pupils pinpoint, minimally reactive, + gag reflex
- Lungs: clear to auscultation bilaterally,
- decreased respiratory rate
- Cardiac: regular rate and rhythm, no
- murmur
- Ext: cool to touch, good pulses, no cyanosis
Clinical Course
A bedside accu-check of “97” was obtained. There were no obvious signs of trauma. Given the patient’s physical exam findings of pinpoint pupils, depressed respiratory rate, and known history of drug abuse, an opioid toxidrome was recognized and the decision was made to administer naloxone. However, with the patient’s poor venous access, an alternative route of administration was required.
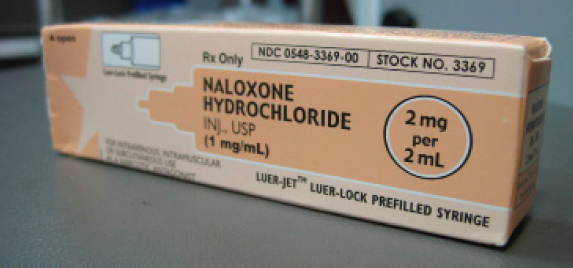
Naloxone
The growing opioid abuse epidemic has resulted in a skyrocketing number of deaths and ED visits for opioid intoxicated patients. According to the CDC, in 2010 opioid analgesics such as oxycodone, hydrocodone, and methadone, were involved in about 3 of every 4 pharmaceutical overdose deaths (16,651)2. Add in the thousands of heroin overdoses and the need for an effective and rapid reversal agent is clear. Administration of intravenous naloxone has been the initial preferred treatment in emergency departments, but may not always be available due to poor venous access. The use of intravenous naloxone is not without risk, and has been associated with unwanted side effects including acute opioid withdrawal, emesis, diarrhea, and agitation. There is also a theoretical catecholamine surge induced by acute opioid withdrawal resulting in pulmonary edema.3,4,7
The safety and difficulty of placing an IV in this specific patient population makes a nebulized route of administration a more efficacious choice. Also, as the patient becomes more alert, they are able to remove the non-rebreather mask themselves, making it a self-titratable medication and limiting the number of undesirable side effects associated with this antidote. Other possible routes when access is lacking include subcutaneous, intramuscular, and intralingual9; although these routes result in sporadic onset of actions.
Nebulized naloxone was first described in a case report in 2003 by Mycyk et al in Chicago5. The patient received the medication via this route due to an inability to gain intravenous access. The nebulized naloxone “gently and effectively reversed the intoxication” without evidence of side effects in that particular patient.
Two recent published studies have further evaluated the use of this intervention. Weber et al8 retrospectively studied 105 consecutive cases of nebulized naloxone administrations over a 5 month period. The primary outcome studied was patient response (a subjective measure). Twenty three (22%) had complete response, 62 (59%) had partial response, and 20 (19%) had no response. No case required assisted ventilation, and no adverse events were documented by paramedics in the prehospital setting. They concluded that nebulized naloxone was a safe and effective alternative although these result in sporadic onset of actions.
In 2013, Baumann et al published a prospective study1 enrolling 26 patients who had a self-reported or suspected opioid intoxication and a spontaneous respiratory rate ≥6 breaths/minute. The primary outcome was level of consciousness, which was recorded pre and 15 minutes post naloxone administration using the Glasgow Coma Scale (GCS) and the Richmond Agitation Sedation Scale (RASS). After nebulized naloxone administration, median GCS improved from 11 to 13. Median RASS improved from -3.0 to -2.0. With “few adverse effects” documented, the authors concluded that nebulized naloxone was “well-tolerated and led to a reduction in the need for supplemental oxygen and results in improvements in GSC and RASS scores”.
Dosing
All of these studies have utilized the dosing of 2 mg of naloxone mixed with 3 ml of normal saline for a total of 5 ml. This solution is then placed in the standard canister and nebulized. Repeated or continuous nebulizers may be required depending on the amount and type of opioid ingested. For example, methadone dosing may require repeated doses of naloxone due to a longer half-life and duration of effect.
Disposition
If the patient is intoxicated to the point that they are failing to ventilate appropriately, intravenous or intramuscular dosing of naloxone still remains the initial treatment. However, since the majority of opioid overdoses present to emergency departments with mild to moderate toxicity, nebulization of naloxone may be the quickest and safest route of administration.
Case Outcome
The patient’s GCS improved from an 8 to 14 within minutes of being placed on 2 mg of naloxone mixed with 3ml of saline in a nebulizer mask. He soon removed the mask himself and had minimal clinical side effects. The patient was discharged 4 hours later after tolerating oral fluids and a turkey/cheese sandwich. No intravenous access was obtained or necessary.
Editor’s Note
The recent Baumann study is the best to date on this new and potentially useful intervention. But they weren’t allowed to randomize their trial; their workup and treatment had to be based on physician preference. Less than 40% of twenty-six patients who got the drug had confirmatory urine testing, and yet just over 40% needed repeated administration. As the original Mycyk paper and prehospital papers suggest, however, in a patient with difficult access, nebulized naloxone’s rapid onset, potentially self-limited dosing, and comparatively milder adverse reactions make it a reasonable intervention to try while attempting to pursue IV naloxone. It’s been ten years since this benign therapy was described, and in this era of opioid abuse, we could probably try nebulized naloxone more often than we do.
REFERENCES
1. Baumann BM, Patterson RA, et al. Use and efficacy of nebulized naloxone in patients with suspected opioid intoxication. Am J Emerg Med. Jan, 2013.
2. CDC Quickstats. “Opioids drive continued increase in drug overdose deaths”. 2.20.13 www.cdc.gov/media/releases/2013/p0220_drug_overdose_deaths.html
3. Flacke JW, Flacke WE, Williams GD. Acute pulmonary edema following naloxone reversal of high-dose morphine anesthesia. Anesthesiology1977;47:376–8.
4. Harrington LW. Acute pulmonary edema following use of naloxone: a case study. Crit Care Nurs1988;8:69–73.
5. Mycyk MB, Szyszko AL, Aks SE. Nebulized naloxone gently and effectively reverses methadone intoxication. J Emerg Med. 2003 Feb;24(2):185-7.
6. Sadove MS, Balagot RC, Hatano S, et al. Study of a narcotic antagonist – n-allyl-noroxymorphone. JAMA1963;183:666
7. Taff RH. Pulmonary edema following naloxone administration in a patient without heart disease. Anesthesiology1983;59:576–7.
8. Weber JM, Tataris KL, et al. Can nebulized naloxone be used safely and effectively by emergency medical services for suspected opioid overdose?. Prehosp Emerg Care. 2012 Apr-Jun;16(2):289-92
9. Maio RF, Gaukel B, Freeman B. Intralingual naloxone injection for narcotic induced respiratory depression. Ann Emerg Med 1987; 16 : 572-577.



1 Comment
what wasn’t Narcan given via IM or Nasal Mist?
J.Toto, RRT, EMT-P