Point-of-care ultrasound is a low-risk diagnosis technique for children with abdominal pain.
This time will be different. “Doctor, I have the surgery resident on line 1 for you.” You present your case: “I have an 8-year-old male who I believe has appendicitis. He experienced the onset of periumbilical abdominal pain about 12 hours ago. The pain has subsequently migrated to his right lower quadrant during the past four to five hours. He reported one episode of non-bilious emesis about two hours ago but no diarrhea. He also reported markedly increased abdominal pain when the vehicle in which he was riding went over a bump in the road en route to the ED. His exam is significant for right lower quadrant as well as rebound tenderness. I also noted an obturator sign. We’ve given him a fluid bolus, and his WBC, which just returned, was 14.5 with 80% PMNs…”
You were going to continue when the surgical resident interrupts, “What did the CT show? You know I am not coming to see him without a CT.” You have had this conversation so many times you’ve lost count.
Here’s the opportunity for which you’ve waited: “Well, this patient is the grandson of the hospital chief of staff who also believes this is appendicitis. He doesn’t want his grandson to experience the radiation exposure imparted by a CT scan. Because I know you are uncomfortable calling your attending without independent verification, I hoped I could provide you some tangible documentation.”
Speaking quickly you add, “I attended a point-of-care ultrasound class a few months ago to increase my skill for this procedure and have subsequently spent quite a bit of time with our ultrasound technicians improving my recognition and scanning skills. My ultrasound is compelling for appendicitis, similar to his clinical presentation. I have saved these images for you and can include them in the electronic chart.”
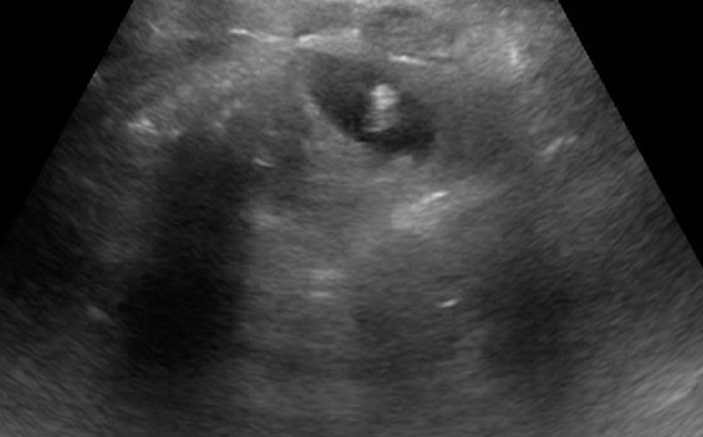
 Figure 1. Transverse and long-axis images of appendicitis. Transverse axis demonstrates a characteristically round structure containing hypoechoic fluid. Noticeable blind-ending loop surrounds the appendix. The long-axis image illustrates a distended blind-ending loop.
Figure 1. Transverse and long-axis images of appendicitis. Transverse axis demonstrates a characteristically round structure containing hypoechoic fluid. Noticeable blind-ending loop surrounds the appendix. The long-axis image illustrates a distended blind-ending loop.
“The ultrasound demonstrates a blind-ending loop measuring about 8 millimeters at the precise point of maximal right lower quadrant wall tenderness (Figure 1 above). There was no visible intraluminal peristalsis of this loop, and it did not compress when I applied direct pressure, pushing it against the underlying psoas muscle. In addition, I noticed considerable inflammation in the adjacent soft tissue” (Figure 2 below).
 Figure 2. Image of appendicitis illustrating surrounding hyperechoic soft tissue suggesting inflammation. Hyperechoic soft tissue is most accurately assessed in the “near-field” so as to not be confused with normal acoustic enhancement that is a normal artifact appreciated immediately posterior to a fluid-filled structure.
Figure 2. Image of appendicitis illustrating surrounding hyperechoic soft tissue suggesting inflammation. Hyperechoic soft tissue is most accurately assessed in the “near-field” so as to not be confused with normal acoustic enhancement that is a normal artifact appreciated immediately posterior to a fluid-filled structure.
Following a short pause, the surgery resident states that he will call his attending. The attending surgeon subsequently makes an appearance in your ED, examines your patient, reviews your images, and discusses the options with the grandfather and the child’s parents. The decision is made to proceed directly to surgery where an enlarged and visibly inflamed appendix is removed. The child’s outcome is excellent and the family is grateful they were spared the delay and radiation involved with a CT scan.
A few days later, you see the surgical resident and thank him for his flexibility. He explains that the attending surgeons are very busy and depend on their residents for direction. In so many words, he communicates that he and his resident colleagues are afraid to be wrong and risk a negative laparotomy. You express your understanding of his situation but mention that his patient’s classic clinical presentation is actually very specific for pediatric appendicitis. However, you convey your understanding that a positive ultrasound is also highly specific when obtained by either a technician in radiology or a trained clinician at the point-of-care. As such, it provides tangible, corroborative and reproducible evidence supporting both the diagnosis and subsequent management. The surgical resident expresses frustration in examining uncooperative pediatric patients whose abdominal discomfort and apprehension frequently cause them to over-state their pain and its distribution. You volunteer to attend the next surgical staff meeting to discuss the use of moderate pre-ultrasound narcotic analgesia intended to enhance communication and hasten sonographic identification of the appendix.
 Figure 3. Long axis view of an enlarged and inflamed appendix.
Figure 3. Long axis view of an enlarged and inflamed appendix.
 Figure 4. Long-axis view of the appendix with a proximal appendicolith with characteristic posterior acoustic shadowing. Adjacent hyperechoic soft tissue
Figure 4. Long-axis view of the appendix with a proximal appendicolith with characteristic posterior acoustic shadowing. Adjacent hyperechoic soft tissue
Key Teaching Points
- Appendicitis is the most common non-traumatic surgical emergency occurring in children. Unfortunately, subtle and atypical presentations are common while traditional clinical evaluation is inadequate to prevent indeterminate or falsely negative assessments.
- The use of computed tomography for patients suspected of appendicitis markedly increases sensitivity but involves exposure of children to ionizing radiation. Ultrasound evaluation, whether provided in radiology or by trained clinicians, markedly increases sensitivity without compromising specificity, and does so without ionizing radiation.
- The presence of absence of various features of appendicitis can be assessed using ultrasound. These can be categorized as (1) direct versus indirect and (2) dynamic versus static. Direct signs provide information regarding the suspected appendix itself. These include static assessments of diameter greater than 6 millimeters, as well as a round shape in transverse axis that appears as a blind-ending loop in the long axis (Figure 3 above). An additional, and highly specific direct sign, is the presence of a hyperechoic appendicolith (Figure 4 above). Certain direct signs are obtained via a dynamic interaction involving the patient, the appendix and the ultrasound probe. Diagnostic certainty is improved when the diseased appendix is visualized as an enlarged, non-compressible tubular structure at the precise site of maximal abdominal wall tenderness. Another highly specific direct and dynamic sign for appendicitis is the observed absence of intraluminal peristalsis within the suspected diseased loop. Indirect signs describe the area in the vicinity of the suspected diseased appendix. These include the presence of hypoechoic fluid/edema surrounding the inflamed appendix and an inflamed, hyperechoic muscularis propria. An inflamed appendix may also be surrounded by prominent, hyperechoic pericecal fat.
- It is important to remember that many of these sonographic evaluations involve the application of pressure to the abdomen of young children. The clinician is most-certainly “on the clock” in regard to the amount of time children will tolerate an ultrasound probe pushing on the abdominal wall. Many clinicians find it expedient to first locate the precise point of maximal tenderness using fingertip palpation prior to applying the ultrasound probe to the point of maximal abdominal wall tenderness. An ultrasound survey of the entire right-lower quadrant can be conducted if the appendix is not located at the point of maximal tenderness. Our experience is that the provision of intravenous fentanyl, one microgram per kilogram (to a maximum absolute dose of about 75 micrograms), approximately 10 minutes prior to sonography, is extremely useful in enhancing patient tolerance of examination without impairing patient-clinician communication. Patient assistance in identifying the precise point-of-maximal abdominal tenderness assists the sonographer’s search for the appendix. Subsequent sonographer-patient communication facilitates the dynamic evaluation.
- Although the addition of ultrasound to clinical evaluation increases sensitivity for appendicitis, there will be cases where the appendix is not visualized. Not all is lost. Staged protocols provide for the use of CT or MRI in situations where uncertainty persists following clinical and ultrasound evaluation. In addition, the sensitivity of ultrasound increases with disease progression and a short waiting period used for a stable patient without signs of peritonitis, followed by a repeat point-of-care ultrasound, may allow subsequent visualization of appendicitis. In this type of situation, we will identify and then interrogate hyperechoic areas, searching for the proverbial appendix-in-a-haystack. In view of the remarkable improvements in image resolution in mobile units, we believe the case for the future use of point-of-care ultrasound for suspected appendicitis is compelling.
- In the current case, the clinical presentation and examination were compelling for appendicitis but the resident’s desire for corroborating independent evidence caused him to request the faithful CT for confirmation. In recent studies, emergency physician-performed bedside ultrasound has consistently achieved specificities above 90%, almost equal to that achieved by CT and sufficient to effect surgery in patients at low risk of perforation.