Treatment options exist – clinical trials and therapeutic guidelines not so much.
A 42-year-old male presented with right flank pain for one day. He denied having a fever and reported a normal appetite. After urinating in the morning, he felt like he couldn’t completely empty his bladder. Past medical history was significant only for hypertension.
CBC and BMP were unremarkable; specifically, the WBC was 8. Urine revealed trace bacteria but no blood and was otherwise negative. A non-contrast CT abdomen/pelvis showed “no ureteral calculus or other acute process.” After his pain resolved, he was discharged.
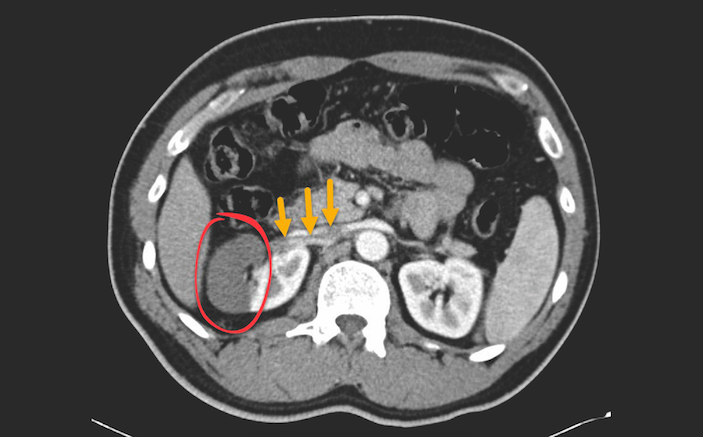
The patient returned six hours later with persistent and worsening right flank pain that radiated to the front. On exam, he has right lower quadrant tenderness, but no guarding or rebound. His GU exam is unremarkable. His WBC is now 13; given the new exam findings, absence of visualization of the appendix on the initial scan, and concern for mesenteric ischemia, a CT abdomen/pelvis with IV contrast is ordered (see image).
The CT shows segmental infarction of the right kidney due to focal arterial occlusion. The incidence of acute renal infarction has been reported as 7 in 100,000. In fact, it was found in 1.4% of cases in an autopsy study – in those cases the diagnosis was made 0.014% of the time. Simply put, it’s a rare disease that is frequently missed [1].
Renal infarction is most often diagnosed in elderly patients; the average age affected is 67 years [2]. Presentations vary widely, but in general, patients complain of flank pain or upper abdominal pain that may be associated with nausea and vomiting. Fever can also be present. On the other hand, patients may be completely asymptomatic and the infarction diagnosed incidentally by CT [3].
Causes of Renal Infarction
There are three primary causes of renal infarction: thromboembolism, in-situ thrombosis, or vascular injury (typically due to trauma). One study gathered retrospective data from 438 patients at nine hospitals with renal infarction diagnosed by imaging studies over a 20-year period. They categorized the etiology as cardiogenic, traumatic (renal artery injury), thrombotic (hypercoagulability), or idiopathic. The most common cause of renal infarction was cardiogenic, accounting for over 50% of cases. Of the remaining cases, 30% were idiopathic, 7% were due to renal artery injury, and 6% were due to hypercoagulability [4].
Since symptoms are so non-specific, diagnosis requires a high degree of suspicion. The most common misdiagnosis is “renal colic.” Urinalysis is not very helpful: patients with renal infarction may have hematuria, proteinuria, both, or neither. Labs are also of little utility in making the diagnosis. Surprisingly, an elevated lactate dehydrogenase (LDH), while highly nonspecific, may be the most useful marker. An elevated LDH is particularly helpful when it is increased more than two to four times the upper limit of normal with normal aminotransferases [5].
One study retrospectively looked at 20 adult patients with renal infarctions. All had either abdominal or flank pain and tenderness. Nineteen patients had an elevated LDH level, and sixteen presented with what is sometimes considered the “classic triad”: abdominal/flank pain, elevated LDH level, and proteinuria [6].
Cortical Rim Sign
A non-contrast CT will fail to make the diagnosis in most cases, but it is almost universally ordered first to exclude other more common diagnoses. Contrast-enhanced CT carries a sensitivity of about 85%. The classic CT finding is the “cortical rim sign”: a 1-3mm rim of subcapsular enhancement paralleling the renal margin as a result of preserved perfusion of the outer renal cortex by capsular perforating vessels [7].
In one study of patients who had a normal non-contrast CT, obtaining a second contrast-enhanced CT led to the correct diagnosis of renal infarction in 50% of cases during the first visit to the ED [6].
Renal infarction is a serious cause of acute nephron loss that is potentially reversible by reperfusion therapy. Unfortunately, due to a paucity of cases there are no good trials or therapeutic guidelines dictating ideal management. The three options for treatment of renal infarction are anticoagulation, thrombolysis, or angioplasty. The decision is in part based upon the duration of symptoms; many cases go undiagnosed for more than 48 hours after the initial presentation. When the underlying cause is a thrombus or hypercoagulable state, anticoagulation is clearly indicated. In the absence of contraindications, initiating heparin and warfarin for 3-6 months is generally accepted as standard of care. Patients should be instructed to take aspirin indefinitely thereafter. Thrombolysis, thrombectomy, and angioplasty are limited by the severity and duration of ischemia. Due to frequent delays in diagnosis as well as a limited number of cases, there is no accepted treatment guideline for when these options should be considered. An atrophic kidney on the affected side suggests prolonged ischemia and less potential benefit with correcting the occlusion. All cases should be discussed with the surgeon and/or interventional radiologist.
Patients suffering from renal infarction may also become hypertensive due to increased renin production. As a result, blood pressure is best treated using ACE inhibitors or ARBs as first-line agents.
The prognosis of acute renal infarction is determined by the etiology and size of the infarct. In most cases of unilateral disease, there is not a significant loss of kidney function; in many instances of bilateral infarct, complete loss of renal function follows.
REFERENCES
- Domanovits H et al. Acute renal infarction. Clinical characteristics of 17 patients. Medicine (Baltimore). 1999;78(6):386-394.
- Lopez VM, Glauser J. A case of renal artery thrombosis with renal infarction. J Emerg Trauma Shock. 2010;3:302.
- Bande D, Abbara S, Kalva SP. Acute renal infarction secondary to calcific embolus from mitral annular calcification. Cardiovasc Intervent Radiol. 2011;34:647–649.
- Oh et al. Clinical characterstics and outcomes of renal infarction. AJKD. 2016;67(2):243–250.
- Winzelberg GG et al. levation of serum lactate dehydrogenase levels in renal infarction. JAMA 1979; 242:268.
- Huang CC et al. ED presentations of acute renal infarction. Am J Emerg Med. 2007;25(2):164-169
- Suzer O et al. CT features of renal infarction. Eur J Radiol. 2002;44:59–64.



1 Comment
Been there done that December 22nd through December 28th. The Doctors at Methodist West and the paramedics that took me to Methodist in Des Moines, IA and the doctor’s at Methodist Des Moines, IA I am so thankful for finding my with a contrast CT with dye and everything was done right in my case. God bless all those who saved my life.