This case has been nine years in the making. In 2000, The Patient Health Information and Quality Act of 2000 required the New York Health Department to collect information and create individual profiles for licensed physicians “in a format that shall be available for dissemination to the public.” These profiles were required to include information on board certification. In 2001 the department defined board certification as “a specialty or subspecialty in which a physician is certified” by various medical specialty board associations. Although a broad definition, AAPS never made this cut as a medical specialty board. As a result, the AAPS certification was excluded on New York’s publicly available physician profile database.

According to the lead defendant, Robert Barnett, Director of the Office of Health Care Quality and Safety, the decision to exclude the AAPS certification came originally on recommendation by the Federation of State Medical Boards, a national organization representing the 70 medical boards of the United States. When asked to change this regulation, Barnett declined, citing the discrepancy in certification requirements between the AAPS and other emergency medicine specialty board association. Specifically at issue was the lack of a residency requirement. In place of a residency, AAPS offers emergency physicians a practice track; any physician who has completed five years of practice in emergency medicine and has passed the AAPS exam can be recognized as a specialist. When Barnett sought the opinion of other medical organizations in New York the answer came back unanimously against allowing the AAPS designation count as “board certified.”
In presenting their argument the AAPS brought forward several physicians who they contended had suffered a professional handicap due to the state’s policy. AAPS held the department responsible for these setbacks and argued that Barnett’s decision to decline AAPS certification was “irrational” and insufficiently rigorous.
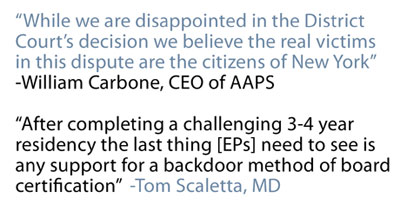
While many specialties have recognized practice-based tracks in the past, the court noted that these tracks closed as available residency slots became sufficient. While some suggest that a shortage of physicians still necessitates the practice track, Tom Scaletta, immediate past president of the American Academy of Emergency Medicine, firmly disagrees.
“The truth is that there are enough emergency physicians,” says Scaletta. “We are in a steep learning curve state with regard to working with scribes and midlevel providers and each can extend emergency physicians by about 50%. We are seeing the market place and national reform effort create more choices for non-urgent cases. So, the non-boarded emergency physicians will have plenty of opportunities to use their primary care certification and desire to deliver unscheduled care.”
While the definition of “board certified” has not changed in New York as a result of this case, Barnett did add a section to the physician profile database called “professional memberships” which emergency physicians can use to list their AAPS specialty certification. In a written statement, William Carbone, CEO of AAPS, called this designation “erroneous” and suggested that the case would be appealed.
“While we are disappointed in the District Court’s decision,” said Carbone, “we believe the real victims in this dispute are the citizens of New York who rely on this website information to make sound physician choices based on accurate and reliable information . . . We believe that AAPS/ABPS will eventually find relief from the discriminatory activities of the State of New York when this decision is more closely examined by a higher court.”



7 Comments
This is why doctors always lose at legislative matters. The arrogance of thinking a midlevel provider is better than a trained physician?? I agree with Mr. Carbone, obviously it’s the people of New York who will suffer.
As the physician shortage worsens, this will eventually be repealed as NY becomes one of the states to not be able to adequately fill it’s ER positions.
It is far more arrogant for a PCP to call him or herself an emergency physician. And, it is far safer for a REAL emergency physician to supervise the care of a minor care patient (what we are talking about when midlevels are utilized in ERs), than for a PCP to be learning about time-sensitive emergencies on-the-job.
ACEP and AAEM have come out STRONGLY against AAPS/BCEM advertising themselves as board certified EPs. Whoever is funding Mr. Carbone’s legal campaign is betting on the wrong horse!
I am an AAPS boarded ER physician since 1995, with 31 years of experience in emergency departments ranging up to 73000 patients yearly. I have supervised er residents in the past at many places,including a major ACEP residency program and most recently a 4th year ER resident from an ACEP residency program who was doing his last rotation with the Indian health service prior to being on his own. I In the former case, they did not know how how to relocate a dislocated mandible which was not fractured and had to call in maxillofacial services to perform what I had done successfully for years in a more rural setting. In the latter case, the soon to graduate 4th year resident was unable to perform a ” difficult” intubation after 2 attempts, I observed him drawing on patients neck in order to perform cricothyroidectomy as I unfortunately was not responsible for supervising him. I intubated the patient after rsi on the first attempt. This brings up 2 points to us ” inglorious bastards” to modern elitist ACEP graduates. Point 1) experience is a much better long term teacher than residency. After all, the father of medicine was practice trained in emergency medicine, as were 25 % of ACEP boarded er docs at 1 time. It is more important to “keep up” over the years as most of what you learn in a few years of residency becomes quickly obsolete. Therefore, I contend that an AAPS boarded er physician who maintains his or her skill at procedures and information by reading and going to AAPS and/ or ACEP procedural and information reviews frequently takes excellent care of his or her patients. In fact , both organizations require lifelong learning cme and testing periodically to assure this. I myself entered residency in 1985 and there were not enough slots at that time in order to accommodate all who wanted to join the club. Therefore, like many of my peers at that time, I opted for 1 year of internal medicine and 1 year family medicine, then left after my father died suddenly and left financial hardship, in order to practice emergency medicine for the next 31 years. An ER residency was not required at that time. Those of us in similar situations have gradually been screwed by the new elitist young pups who brag about their 80 hour per week residency ( when we did 120 or more) as being the only way to know and practice emergency medicine properly. BULL. I was putting in chest tubes and treating major traumas when they were in diapers! I RESENT being forced out of the profession that I love just because I am old (an experienced) and there were too few residency slots when I was young. Evidently 2 years of residency and 31 years of experience are not equivalent to a 3-4 year “rigorous” 80 hour week residency. Again BULL. Point2) Most ER residents are trained in non rural settings, with all the ancillary services in order to “kiss their grits” every time they cant handle something. I have worked in both settings, and the present ACEP graduate depends on these ancillary services. They are lost without a trauma team, orthopedics, cardiology, maxillofacial, cath lab, etc and cannot work effectively without further training in the rural setting, where the need for emergency physicians is greatest. There IS a shortage of rural boarded er physicians for this reason as well as ACEP has shifted the “BIG BUCK” jobs into the cities, drawing most of its graduates to practice there. This comes down to nothing more than a money game. If you do not go to our residency, you will not be eiligible to work where they pay the most. Other residents, the old and more experienced, are excluded for the “ACEP CLUB.”
In 1994-95 I was working for Greg Henry (ACEP-President Elect) as an ER director. I asked his opinion on AAPS and how he will affect the profession. After all, he was practice trained as were most partners in Ann Arbor. He immediately became angry and wanted to know how to interfere with such a certification board.
Now, the virus has created a great need for ER docs, ACEP or AAPS.
In the end the people suffer not the hospitals. Working with the father of ER medicine in HS, I beg to differ with Henry’s stance. ER medicine is a global learning process that takes many skills and supporting tools.
AAPS by the way also requires a residency to take the ER board.
It’s a great example (again) of Ann Arbor being the bully in the BIG 10 and this spills over to healthcare especially in rural America.
While there is certainly a skewed distribution of all physicians, including emergency physicians, the use of physician extenders has made the practice of medicine somewhat easier for doctors and patients. There is no other specialty which has to contend with this ersatz board certification claimed by BCEM; can one imagine someone claiming that 5 years of looking at Xrays qualifies him or her to be a radiologist, or 5 years of looking at ECGs to be a cardiographer? Many of us who have practiced for years had the opportunity to take ABEM or AOBEM boards; when the window closed, those who wanted to become certified by the recognized boards had the opportunity to participate in a recognized residency. Otherwise, anyone can practice emergency medicine, without certification, and there are still a large number of jobs available.
There is no question that a residency trained Emergency Physician is more capable in the ER than a physician without that training early in their career. There is also no question this difference in quality of both physicians blurs over time. Differences in quality become related to their experience and continued education. The status symbol of residency may not be lost in the view of the public and educators, but in reality other factors become more important over time.
My qualifications for this statement: 20 years of full time Emergency Medicine preceeded by 15 years of part-time EM, ABFM since 1977 CAQ Geriatrics, BCEM 1996-2006, still practicing EM.
EM residency trained doctors rarely decide to serve the rural hospitals, where resources are not as available and advanced as they are in their training hospitals. There are hundreds of rural hospitals where no board certified EP has ever shown his/her face, and who works the days and night shifts? – Yes, you guessed it right. Primary Care Physicians!
I completed my residency in Family Medicine (ABFM), and b/c of life challenges, I ended up in rural Australia doing emergency medicine for 5 years. Then I return to the US and worked another 5 years in rural Tennessee. Through out the years, I have completed more than 100 CME hours per year in EM by assisting to meetings (ACEP, USC essentials, High Risk EM, Trauma, Airway and Ultrasound courses, etc) self study programs (EM:RAP, RMM, EMA, journals, etc) and completed AAPS certification 4 years ago.
Board certification opens up opportunities for doctors and patients to have a better health care system in non-urban areas, and quite frankly, the statement that only residency trained EP can be certified is not just wrong but it is also arrogant and without basis.