Answer: Privately-owned submarines. Five tons of cocaine worth over 350 million dollars was discovered in a submarine off the Guatemala coast in 2008.
Educational Objectives:
-Identify issues associated with body packers and stuffers
-Implement different treatment strategies for body packers and stuffers
-Recognize the critical differences between body packers and stuffers
*****************


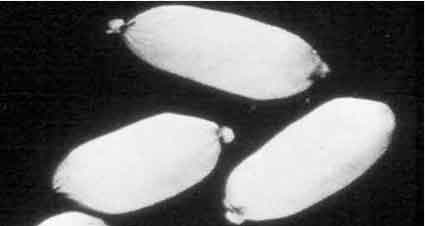
 The physician should attempt to obtain any information regarding the amount of drug ingested and the type of packaging to predict the potential for toxicity. Plain abdominal radiographs are generally not useful for body stuffers, but may be positive with body packers (figure 3). Gastrograffin swallow or CT scan of the abdomen with contrast may reveal ingested packets in cases where plain radiographs are negative, but tend to be nonspecific and reader dependant. ED bedside ultrasonography would be a noninvasive method to rapidly assess for multiple drug packets, particularly in the gastric region.
The physician should attempt to obtain any information regarding the amount of drug ingested and the type of packaging to predict the potential for toxicity. Plain abdominal radiographs are generally not useful for body stuffers, but may be positive with body packers (figure 3). Gastrograffin swallow or CT scan of the abdomen with contrast may reveal ingested packets in cases where plain radiographs are negative, but tend to be nonspecific and reader dependant. ED bedside ultrasonography would be a noninvasive method to rapidly assess for multiple drug packets, particularly in the gastric region.
In body stuffers and packers, gastric lavage is ineffective and contraindicated, as the procedure may cause rupture of the packets. Conservative therapy using polyethylene glycol whole bowel irrigation (WBI) is generally recommended in patients with potential toxicity. The most common product, trade named “GoLytely”, (I challenge anyone to come up with a better medical misnomer) is dosed at 1-2 liters per hour. It often requires NG tube administration unless the patient is cooperative. In patients who are extremely agitated, combative or exhibit violent behavior, WBI should be withheld. Activated charcoal is given prior to whole bowel irrigation to adsorb any leaking drug from the packets. Charcoal noted in the rectal effluent also helps indicate a completed round of WBI. It is important to ensure that all ingested packets are accounted for before the patient is discharged. After cleaning off the charcoal residue, turn any illegal contraband over to hospital security or the proper authorities—for obvious reasons, avoid “pocketing the evidence”. Patients in police custody are particularly high risk for subsequent morbidity due to a lack of reliable follow-up care or means of close observation and monitoring. Body packers with significant toxicity or evidence of bowel obstruction should have a surgical consultation. Laparotomy may be a necessary lifesaving intervention to remove leaking packets.
Body packers or stuffers with heroin or opioid-containing drugs may present with altered mental status, depressed respiratory drive, and miotic pupils. These patients may also require GI decontamination with whole bowel irrigation in order to enhance the elimination of drug packets. Contraindications to WBI include unstable vital signs, respiratory compromise, and lack of bowel sounds or gut motility. In contrast to scenarios involving cocaine, a less aggressive approach to surgical intervention is warranted with heroin packing. Supportive care and antidotal therapy with naloxone may be required for more prolonged periods of time. A recent five year case series from Chicago reported a relatively benign clinical course in most heroin body stuffers. Nine percent of patients developed signs and symptoms consistent with opiate intoxication and only 5% required naloxone administration. The mean observation time in this series was 24 hours.
Other drugs of abuse described in isolated cases of body packers and stuffers include methamphetamines, phencyclidine, cannabinoids and various hallucinogens.
Answer: They were being used as “body packers” to smuggle cocaine into the US from South America.
- Dattilo P, Hailpern S, Fearon K, et al: B-blockers are associated with reduced risk of myocardial infarction after cocaine use. Ann Emerg Med 51(2): 117-126, 2008.
- Eng JG, Aks SE, Waldron R, et al: False-negative abdominal CT scan in a cocaine body stuffer. Am J Emerg Med 17:702-4,1999.
- Goertemoeller S, Behrman A: The risky business of body packers and body stuffers J of Emerg Nursing, Volume 32 (6), 541-544, 2006.
- Hoffman RS: Cocaine and B-blockers: should the controversy continue? Annal Emerg Med 51(2): 127-129, 2008.
- Hoffman RS, Smilkstein MJ, Goldfrank LR: Whole bowel irrigation and the cocaine body packer: a new approach to a common problem. Am J Emerg Med 8(6):523-527, 1990.
- Jordan MT, et al: A recent case series reported nine percent (6/65) of patients developed signs and symptoms consistent with opiate intoxication after oral stuffing of heroin. J Emerg Med. 36(3): 250-256, 2009.
- June R, et al: Medical outcome of cocaine body stuffers. J Emerg Med 1(2):221-224, 2000.
- Olmedo R, et al: Is surgical decontamination definitive treatment of “body packers”? Am J Emerg Med 19(7):593-96, 2001.
- Roberts JR, et al: The body stuffer syndrome: a clandesteine form of drug overdose. Am J Emerg Med 4(1):24-27, 1986.
- Schaper A, et al: Surgical treatment of cocaine packers and body pushers. Int J Colorectal Dis 22(12): 1531-35, 2007.
- Taheri MS, Moharamzad Y, Nahvi V: Abdominal CT findings of ruptured opium packets in a body packer European Journal of Radiology Extra, Volume 70 (1): e21-e23, 2009.
- Traub SJ, Hoffman RS, Nelson LS: Body packing-The internal concealment of illicit drugs. N Engl J Med 349; 26: 2519-26, 2003.
- Utecht MJ, Stone AF, McCarron MM: Heroin body packers. J Emerg Med 159:750-754, 1993.



2 Comments
If patient was admitted for follow up to rule out heart attack and discharge 24 hours later rulling out AMI or MI as a cause. The doctor then refers the patient for a stress test for MI with the Cardiologist. Also discharge diagnosis was chest pain sysdrome but bill my insurance for unspecified chest pain. I have three diffrent diagnosis of my event.
I had stress test performed one month after discharge from hospital which rule out AMI or MI. It has now come to past that I need a Coronary bypass performed because my arterys are block and damage has occurred. I feel that had this procedure been done one month ago when I was admitted perhaps some of the damage could have been prevented.