Tramadol provides suboptimal pain relief, is a high risk for abuse and addiction, has multiple drug-drug interactions and bad side effects. So why in the world is it surging in popularity?
A conversation between Drs. Sergey Motov and Nicholas Genes.
Nicholas Genes: Is it just my imagination, or am I seeing a rise in tramadol prescriptions? It’s not just patients coming into the ED with the prescriptions from other providers – I think I’m seeing my own PAs and residents ordering it in the ED, and prescribing it. Am I imagining this?
Sergey Motov: You are not imagining it. You are witnessing an uncontrolled surge in tramadol prescribing across multiple medical specialties including EDs across the US. For example, between 2008 and 2014, rates of annual tramadol prescribing doubled from 22 million to 44 million [1]. Data from IMS Health’s National Prescription Audit Plus Report demonstrated that between 2009 and 2011 significantly more prescriptions were written for tramadol than for any other opioid other than hydrocodone and oxycodone. In 2012, tramadol outranked oxycodone and became the second most commonly prescribed opioid in the United States after hydrocodone [2]. Similarly, due to laxity of international opioid regulations, tramadol global consumption has increased by 186% from 2000 to 2012 [3]. So, as you can see, tramadol is becoming an increasingly popular opioid analgesic.
Genes: Why should this be? Do they all think it’s a less addictive (or less euphoric) opioid? Or it’s a better pain medication?
Motov: The painful reality is that a misleading marketing campaign in 1995 proclaimed tramadol to be as effective as other opioids but with the lack of risk for abuse and dependency. This was largely overlooked by the FDA, which failed to acknowledge research demonstrating that the oral form of tramadol had similar abuse liability as oxycodone (OxyContin). Because of this misinformation, tramadol was not restricted under the Controlled Substance Act [4]. In the end, this marketing campaign led to virtually uncontrolled prescribing of tramadol. But the truth, based on the post-marketing research, is that tramadol provides suboptimal analgesia, possesses high abuse and addiction risk, has multiple drug-drug interactions, and has an unfavorable (unique) side effect profile [5,6]. As a result of “perceived” safety, the number of tramadol-related ED visits involving misuse or abuse increased about 250 percent from 6,255 visits in 2005 to 21,649 in 2011. The number of tramadol-related ED visits due to adverse effects increased by 300% from 6,207 in 2004 to 25,558 in 2011, and ED visits due to tramadol-related suicide attempts increased by nearly 400% from 1,742 in 2004 and 5,692 in 2011 [6].
Genes: Well then. What is tramadol’s mechanism of action? And how does it compare to other commonly prescribed opioids?
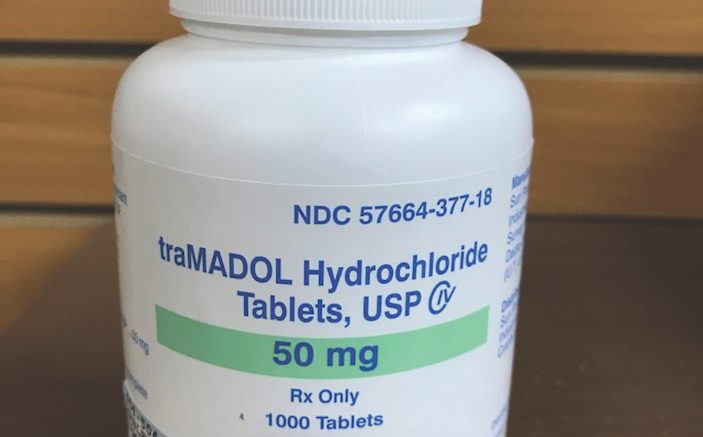
Motov: Tramadol is a central acting synthetic opioid analgesic that is frequently prescribed in the United States to treat a variety of acute and chronic painful conditions. As a racemic mixture, tramadol has dual mechanisms of action: It binds to mu opioid receptors and, simultaneously, blocks the re-uptake of serotonin and norepinephrine. Tramadol’s active metabolite, M1 (O-desmethyltramadol) has higher affinity to mu receptors than the parent drug, but this affinity is approximately 100 times less than that of morphine [7]. This weak opioid agonism results in tramadol having modest-at-most analgesic efficacy. In fact, tramadol administration to patients with acute traumatic musculoskeletal pain resulted in lesser degree of pain relief than acetaminophen/hydrocodone combination [8]. Similarly, a combination of APAP/hydrocodone was found to have greater analgesic efficacy and longer time to re-medication in patients after oral surgery in comparison to APAP/tramadol combination [9].
Furthermore, tramadol was found to result in similar change in pain score as acetaminophen in patients with non-traumatic acute abdominal pain, and lesser degree of pain relief in comparison to NSAID (metamizole) in patients with biliary colic [10,11].
Lastly, a Cochrane review that compared analgesic efficacy of acetaminophen/tramadol combination to either acetaminophen or ibuprofen alone demonstrated superior analgesia of this combination to acetaminophen alone, but similar and even inferior pain relief to 400 mg of ibuprofen. Of note, the acetaminophen/tramadol combination did not result in superior analgesia when it was compared to acetaminophen given at 975 mg per dose [12].
When it comes to euphoria, multiple surveillance reports and data from SAMHSA and DAWN clearly demonstrate a dose-dependent opioid-induced euphoric effects of tramadol that is similar to oxycodone and heroin [2,13]. As an example, Senay et al reported high rates of physical dependence to tramadol based on the surveillance data and even higher rates (about 40%) of typical (opioid-like) and 5-8% of atypical (NE/serotonin) withdrawal symptoms related to abrupt cessation of tramadol use that included hallucinations, paranoia, extreme anxiety, panic attacks, confusion and unusual sensory experiences such as numbness and tingling in one or more extremities [14]. These reports are the reasons that tramadol was finally placed into Schedule IV of the Controlled Substance Act [2].
When tramadol is consumed repetitively and/or for prolonged periods, its use is associated with high risk of addiction. In fact, a report from the Wall Street Journal clearly states that tramadol is the leading cause of opioid abuse and addiction worldwide with the exception of the United States [3]. Once again, the “perceived safety” of tramadol leads to a false belief among doctors and patients that it is less harmful and addictive than oxycodone and oxycontin. In addition, factors that contribute to addiction include ease of obtaining tramadol from hundreds of websites without prescriptions and a cost of as little as $0.12 per tablet. Not to mention, it’s easy to tamper with the extended release capsules, to get instantaneous euphoric effects similar to heroin, but longer-lasting [15].
 Genes: So how bad is tramadol with respect to the adverse effects?
Genes: So how bad is tramadol with respect to the adverse effects?
Motov: Tramadol’s simultaneous opioid agonist action and serotonin (5-HT) and norepinephrine reuptake inhibitory effects result in a unique side effect profile and important drug interactions. To start, tramadol’s opioid analgesic potency is influenced by the individual’s CYP2D6 enzyme genetic polymorphism. In other words, “ultra-rapid” metabolizers have an increased risk of overdose and even death [16].
Tramadol use in higher doses or abuse and overdose are associated with a high rate of neurotoxicity that includes seizures and lethargy due to the blockade of serotonin and norepinephrine re-uptake [17,18]. Of note, several case series and chart reviews pointed out that the minimal tramadol dose that might lead to seizure ranges between 200-500mg [19,20].
Tramadol consumption has a potential to cause hypoglycemia. According to Fournier and colleagues, patients taking tramadol had higher risk of hypoglycemia requiring hospitalization in comparison to patients taking codeine. Interestingly, that risk was the highest in the first 30 days of tramadol use [21]. In addition, tramadol use for the first 30 days is associated with 2-3-fold increased risk of hospitalizations for hyponatremia in comparison to codeine [22].
When tramadol is used or abused in combinations with selective serotonin re-uptake inhibitors and tricyclic antidepressants, the serotonergic effects are enhanced that lead to development to serotonin syndrome with occasional lethal outcomes [23]. Thus, it is imperative to EM clinicians to not to prescribe tramadol to patients taking agents that increase serotonin concentrations, or at least execute extreme caution [24].
Genes: Yeesh. Beyond the adverse effects, though, there are some patients that swear by it. I get that it’s unpredictable, but if a patient comes in on tramadol and it’s helping their pain, should I recommend a different med, or leave well enough alone? Is long-term use a risk? What drug-drug interactions should I worry about?
Motov: Patients on long-term opioid therapy that includes tramadol represents the greatest challenge to EM clinicians. We should make a real effort in discussing risks of long-term tramadol use with referrals to an addiction specialist who can assist in weaning off or replacing this opioid analgesic by enrolling into medication-assisted therapy (MAT) programs with buprenorphine as an example. You should not abruptly stop patients from taking tramadol as withdrawal is associated with severe morbidity. Long-term use of tramadol has a high risk of leading to addiction.
Genes: You’ve talked a lot about alternatives to opioids (like topical meds in our last interview, or superior NSAID prescribing earlier this year). But if we do decide to prescribe an opioid, what should it be? Percocet? Vicodin?
Motov: I am a big proponent of morphine sulfate immediate release (MSIR) tablets for acute pain in the ED and at discharge. Limited research demonstrates similar analgesic efficacy of MSIR in comparison to hydrocodone and oxycodone but significantly lower rates of likeability (euphoria) and abuse liability (recreational use) [25]. In addition, several randomized controlled trials that included morphine failed to demonstrate statistically significant abuse potential or reinforcing effects of morphine [26-28]. When morphine was given in high doses, it was found to have predominantly dysphoric effects and increased negative side effects that included dry mouth and flushing [27,28]. Furthermore, “take again” and to be “wanted” rating for morphine were less likely than placebo [28]. The MSIR is available in tablets and liquid form with dosing ranging from 10 to 15 mg per dose for opioid-naïve patients. The only limiting step in prescribing of MSIR is a lack of availability in many local pharmacies.
REFERENCES
- Drug Abuse Warning Network Report May 14, 2015. Accessed on 10/13/17. https://www.samhsa.gov/data/sites/default/files/report_1966/ShortReport-1966.html
- Diversion Control Division Report. Federal Register Volume 78, Number 213 (Monday, November 4, 2013). Accessed on 10/13/17 https://www.deadiversion.usdoj.gov/fed_regs/rules/2013/fr1104.htm
- Tramadol: The Opioid Crisis for the Rest of the World. The Wall Street Journal. Accessed on 10/13/17. https://www.wsj.com/articles/tramadol-the-opioid-crisis-for-the-rest-of-the-world-1476887401
- Drug tramadol escapes stricter regulation.Watchdog report, JSOnline, 12/21/13. Accessed on 10/13/15. http://archive.jsonline.com/watchdog/watchdogreports/drug-tramadol-escapes-stricter-regulation-b99158486z1-236900801.html/
- Three Reasons Not to Prescribe Tramadol by DeLaney M. 05/04/2015. Accesed on 10/13/17. http://empharmd.blogspot.com/2015/05/three-reasons-not-to-prescribe-tramadol.html
- Emergency Department Visits For Adverse Reactions Involving The Pain Medication Tramadol. The CBHSQ Report 10/14/2015. Accessed on 10/13/17. https://www.samhsa.gov/data/sites/default/files/report_1965/ShortReport-1965.html
- Grond S, Sablotzki A. Clinical pharmacology of tramadol. Clin Pharmacokinet. 2004;43(13):879-923.
- Turturro MA, Paris PM, Larkin GL. Tramadol versus hydrocodone-acetaminophen in acute musculoskeletal pain: a randomized, double-blind clinical trial. Ann Emerg Med. 1998 Aug;32(2):139-43.
- Fricke JR Jr, Karim R, Jordan D, Rosenthal N. A double-blind, single-dose comparison of the analgesic efficacy of tramadol/acetaminophen combination tablets, hydrocodone/acetaminophen combination tablets, and placebo after oral surgery. Clin Ther. 2002; 24:953-68
- Oguzturk H, Ozgur D, Turtay MG, Kayaalp C, et al.Tramadol or paracetamol do not effect the diagnostic accuracy of acute abdominal pain with significant pain relief – a prospective, randomized, placebo controlled double blind study. Eur Rev Med Pharmacol Sci. 2012 Dec;16(14):1983-8.
- Schmieder G, Stankov G, Zerle G, Schinzel S, et al. Observer-blind study with metamizole versus tramadol and butylscopolamine in acute biliary colic pain. Arzneimittelforschung. 1993 Nov;43(11):1216-21.
- Edwards JE, McQuay HJ, Moore RA. Combination analgesic efficacy: individual patient data meta-analysis of single-dose oral tramadol plus acetaminophen in acute postoperative pain. J Pain Symptom Manage. 2002; 23:121-30
- Is Tramadol the New OxyContin? DrugAbuse.com. Accessed on 10/13/17. https://drugabuse.com/library/is-tramadol-addictive/#is-tramadol-as-addictive-as-oxycontin-
- Senay EC, Adams EH, Geller A, Inciardi JA, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend. 2003 Apr 1;69(3):233-41.
- Will Tramadol Addiction Overtake OxyContin Addiction? NovusDetox. Accessed on 10/13/17. https://novusdetox.com/oxycontin-tramadol-addiction-abuse.php
- Miotto K, Cho AK, Khalil MA, Blanco K, et al. Trends in Tramadol: Pharmacology, Metabolism, and Misuse. Anesth Analg. 2017 Jan;124(1):44-51.
- Gardner JS, Blough D, Drinkard CR, Shatin D, et al. Tramadol and seizures: a surveillance study in a managed care population. Pharmacotherapy. 2000 Dec;20(12):1423-31.
- Labate A, Newton MR, Vernon GM, Berkovic SF. Tramadol and new-onset seizures. Med J Aust. 2005 Jan 3;182(1):42-3.
- Marquardt KA, Alsop JA, Albertson TE. Tramadol exposures reported to statewide poison control system. Ann Pharmacother. 2005 Jun;39(6):1039-44. Epub 2005 May 3.
- Spiller HA, Gorman SE, Villalobos D, Benson BE, et al. Prospective multicenter evaluation of tramadol exposure. J Toxicol Clin Toxicol. 1997;35(4):361-4.
- Fournier JP, Azoulay L, Yin H, Montastruc JL Tramadol use and the risk of hospitalization for hypoglycemia in patients with noncancer pain. JAMA Intern Med. 2015 Feb;175(2):186-93
- Fournier JP, Yin H, Nessim SJ, Montastruc JL, et al. Tramadol for noncancer pain and the risk of hyponatremia. Am J Med. 2015 Apr;128(4):418-25.e5.
- Sansone RA, Sansone LA.Tramadol: seizures, serotonin syndrome, and co-administered antidepressants. Psychiatry (Edgmont). 2009 Apr;6(4):17-21.
- Nelson EM, Philbrick AM. Avoiding serotonin syndrome: the nature of the interaction between tramadol and selective serotonin reuptake inhibitors. Ann Pharmacother. 2012 Dec;46(12):1712-6.
- Wightman R, Perrone J, Portelli I, Nelson L. Likeability and abuse liability of commonly prescribed opioids. J Med Toxicol. 2012 Dec;8(4):335-40.
- Zacny JP. Characterizing the subjective, psychomotor, and physiological effects of a hydrocodone combination product (Hycodan) in non-drug-abusing volunteers. Psychopharmacology. 2003;165(2):146–156.
- Zacny JP, Gutierrez S, Bolbolan SA. Profiling the subjective, psychomotor, and physiological effects of a hydrocodone/acetaminophen product in recreational drug users. Drug Alcohol Depend. 2005;78(3):243–252.
- Zacny JP, Lichtor SA. Within-subject comparison of the psychopharmacological profiles of oral oxycodone and oral morphine in non-drug-abusing volunteers. Psychopharmacology. 2008;196(1):105–116.



12 Comments
I’d like to hear more on why the authors suspect the data on MSIR is so favorable. I was surprised by such positive data mentioned in the article.
Doctors Genes and Motov..
Thanks for an excellent review of tramadol….now a few words as to “why in the world is it surging in popularity”. A clue as to my longevity is I remember well Zomax as the pain-ending-NSAID-to beat-all-NSAIDs, the brilliant marketing of “Percogesic” as an OTC pain med, the pandering of oxycontin reps and the rock hard buttocks of migraine Demerol’ers (called in by PCP’s to the “emergency room” ) and the explosion of the opiate crisis in the USA, now a “Presidential-endorsed National Emergency”. I practiced overseas for 12 years and learned rational and humane pain management that did not include Rx’s for narcotics for every moan and groan, use of IV acetaminophen and diclofenac and others. Now, back to the grind here, I am bombarded on one hand with demanding,needy, irate, chronic pain patients (one of whom has a complaint against me in the Medical Board for not giving her Dilaudid-on-demand with a clear history of opiate habituation and addiction which I discovered from consulting (mandatory in State) the Prescribing Monitoring System, and then charged with a HIPAA violation for talking about it with her mother in the room despite her permission. Not to mention shortages of most other pain meds, no stocking of alternatives, unethical primary docs being “candy” dispensers , pharmacy restrictions limiting you to 3-4 days of pain meds (i.e.. repeated ED visits) and hospital Administrators who absolutely refuse to take a stand in their communities to stop advocating folks coming to the ED expecting opiates. The result: more tramadol prescriptions, an admittedly awful drug, still fraught with the risk of addiction/misuse, seizures and confusion in old folks etc. etc. as your discussion points out, and …it doesn’t work very well. However, exactly what are the alternatives? An NSAID? The patient is or states they are allergic or increasingly on anticoagulants or have bad kidneys. Sub anesthetic ketamine? Great, and I use it regularly for certain conditions, but not all that applicable as a general analgesic. Compazie or Reglan/Benadryl for migraines?…always. Morphine MSIR ? Not worth the phone call from the pharmacy which doesn’t carry it anyway or the prescription monitoring report I get every 3 months. Hydrocodone, oxycodone, hydromorphone, oxycontin?? Got us into the problem to begin with. So, doctors, I have made a conscientious effort to be humane (I’m a procedural sedation Meister), and truly manage acute painful conditions but the reality of our approach in the ED to pain management is we are caught in a malestrom of “a national emergency” of opiate use, a politically charged directive which loves to finger point at providers and a populace of medical consumers that make unreasonable demands of us/their health system and hospitals and management groups that value Press Gainey above ethical sound medical decision making.
I will take the tramadol as the not-really-lesser-evil.
I believe you are working for the drug company I have tramadol a long time through veterans administration, funny now I labeled a drug seeker, put me on pain contract. the reason I opted for chronic pain because doctors were giving vicodin like candy. I want to minimalize my pain while im at work in emergency room during the day, if pain is not controlled by pepper cream I may take a narco so that I rest for work. I believe this is a joke that tramadol being new oxy. I believe drug company may be selling more drugs for drug seeker to try the new oxy but that wont last long. like saying Darvon is new fentanyl. I believe the federal government thinks they are saving drug addicts from death, so they invented pain contract to manage drug use. what a fairy tale! this is another attempt to give control to all veterans, natives ,welfare people. Having someone to give my meds I don’t even know and do not know me
It seems that the present state of industrializing medicine with its claim that ‘customers deserve to be pain free’ has forgotten–or refuses to acknowledge–that most of us trained before the ‘customer-right to be pain free age’ (see the West Virginia and JCAHO lawsuit page that I also commented on) were taught that it’s not the pie-in-the-sky ‘pain free right’ that has been policy-implemented over the past couple of decades that medicine was responsible for but the requirement in medicine to teach each patient how to manage his or her pain–not ‘completely remove it’ as these policies claim. While, especially in chronic pain patients, I don’t see that within the purview of ED physicians, I do try to implement sequential pain control in patients–including topical treatments, NSAIDS, acetaminophen, etc–however, especially with the implementation of policy-implemented ‘right to be pain free’ mandates, I do add a narcotic with the stipulation ‘and IF NEEDED, can resort to this’ more as the last resort, not the first treatment. But, a couple of statements to make with regards to this issue of Tramadol: First, I practice in the state of Texas and Texas has recently placed Vicodin in the Schedule II category requiring triplicate prescriptions in the state of Texas which, as an ED physician, I refuse to carry (since it really is hard to determine just how much pain especially a chronic pain patient has when they come to the ED as I remember my own neurology-mentor in medical school stating that ‘there will always come a time in treating chronic pain with narcotics when you will wonder if you are treating their pain or their narcotic addiction’ and I don’t want them coming back to me for their Schedule II drug fix)–plus, it is a hassle to have to keep track of triplicate prescription drug applications with State Board supervision implications in a person that you only sporadically see (and if you are seeing them recurrently in the ED for the same pain, something’s wrong with how their care is being implemented elsewhere, anyway). Secondly, since I do try to implement pain-relief sequentially using non-narcotics methods first, and since that implementation frequently involves using both NSAIDS and acetaminophen, Tramadol has become my ‘go-to additive’ of recent because it has neither NSAIDS nor acetaminophen mixed with it–so it can be ‘added to’ the previous suggested management IF NEEDED. What other alternative do I have? All the others, as mentioned above, have either gone by the wayside or require the triplicate prescriptions in Texas that, as an ED physician, I don’t want to carry.
I have to admit that I quit reading your comment after the early sentence about chronic pain patients deserving pain free living (or not, in your narrow minded opinion. Have some severe chronic pain for a few years, or so, and get back to us. I have had severe psoriatic arthritis singe age 23; I suffered with non-optimal treatments until 40, while working and raising a family after grad school. In my early forties I started gold, the a small oral dose of methotrexate that I felt were miracle drugs. At 50. I started injected methotrexate and the miracle was complete…now I am on dialysis with destroyed kidneys, and the arthritis meds I can afford no longer work, and methotrexate is contraindicated with dialysis.
So please try my excruciating, minute by minute, daily pain for awhile and repeat your lame claim. Tramadol 50 mg twice. Day barely touches the pai. If anything, 5 mg oxy is less helpful and I awake with a miserable sore throat.
I think this article is bullshxx. As a person in the medical field whp worked in busiest er in Las Vegas, and also having first hand knowledge of this med. O have seen many pain med addicted patients daily. 3oit of 5 patient/day are pain med seeking from addiction. Not one patient has ever been admitted for over dose from tramadol. Nor has anyone come in begging for tramadol. People who take it are never given more than 100mg in a dose . None of the people I see have ever felt the need to take 200-500mg in a dose. So yes it can be habit forming and body becomes dependent, but taking it as prescribed 100-300mg /day has not had any issues you claim it does, except withdrawal symptoms are horrific. Yes it is dangerous to abruptly stop. So don”t stop it. Patient w/ chronic pain find it very useful. Only complaints are nausea and unable to sleep/ racing thoughts….. UNLIKE morphine or lortab most problematic drug in this country that patients die from having the desire to tale as many as they can get ,,,,,,,,and stop breathing. The are not any death recorded from a healthy person by just taking 100-300mg/day. There is millions of cases where a healthy patient dies after taking small amounts of true opioids. Never seen or heard of any patient being admitted for tramadoi ever, ONLY patients who have taking med for a long time cone to ER after they has cut off meds and need med to stop or prevent horrific withdrawal.ONLY people that read articles like this and think this is fact have caused more ppl to die from being prescribed more opioids instead of trying tranadol as a safer alternative
WOW, I’m sorry to tell u this, but you are DEAD WRONG ABOUT TRAMADOL!! And I don’t know where your getting your information, but you really need to do your homework, before you come on a blog like this one, and make yourself look STUPID!! While reading your post, I just kept thinking to myself, that “MAN, THIS PERSON DOESNT EVEN KNOW WHAT THEIR TALKING ABOUT “!! EXTREMELY IGNORANT “!! And I know, because I could be the freakin POSTER CHILD FOR TRAMADOL ADDICTION, and I am currently in a lawsuit against the makers of Tramadol, because they ultimately DESTROYED MY LIFE!! And all you have to do is jump on the internet, and type in Tramadol overdoses and DEATHS, and you’ll find tons of articles about the devastation it has caused, because they didn’t do the proper trial with the FDA, and marketed and pushed it to doctors as a NON NARCOTIC, and NON ADDICTIVE, and then after ruining THOUSANDS OF LIVES , ADMITTED WRONG DOING, because they didn’t put proper warning labels on it, and I’ve NEVER BEEN A DRUG ADDICT, and I was prescribed 240 a month, following wrist surgery, and I was a FLIGHT ATTENDANT , and told the doctor that I needed something for pain, but DID NOT WANT ANY NARCOTICS, and he told me that there is a drug called Tramadol/Ultram, that works GREAT FOR PAIN, but has NO NARCOTICS, and doesn’t make you high!!! And long story short, is that I ended up becoming EXTREMELY ADDICTED, after four years, before it being changed to a scheduled OPIOID NARCOTIC, and ANOTHER 3 years trying to get help, and am now on SUBOXONE AND COUNSELING!! The withdrawals were EQUAL TO HEROIN WITHDRAWALS!! It’s been a FREAKIN NIGHTMARE!! DESTROYED MY LIFE!! RELATIONSHIP, FINANCES, HEALTH ETC!! TRAMADOL IS PART OF THE NATIONAL OPIOID CRISIS, So the next time you wanna get on the internet and post your opinion on a topic, you might wanna make sure you brush up your knowledge on the subject!! Because for the thousands of people who have suffered from addiction to Tramadol, and the families who have lost loved ones to this drug, it’s a real SLAP IN THE FACE!! And extremely inconsiderate!!!! So next time DO YOUR HOMEWORK, or talk about a topic you actually DO KNOW SOMETHING ABOUT!!
Great point could you email me I have a question Angela @. a1chevy64@gmail.com please thanks
And to add to my comment above, as I just remembered your occupation, and am STUNNED THAT YOU EVEN WORK IN A FREAKIN HOSPITAL AND YOU ARE THAT IGNORANT ABOUT TRAMADOL? How can you work in a freakin hospital and NOT KNOW ABOUT HOW BAD TRAMADOL IS? Or about the THOUSANDS OF PEOPLE ADDICTED TO IT? And all the DEATHS FROM IT?!! And you absolutely DO NOT NEED TO BE ON IT A LONG TIME TO BECOME ADDICTED!! In fact it causes bad withdrawals after only ONE WEEK OF TAKING IT!!! So you, my friend, were DEAD WRONG ON EVERY DETAIL OF YOUR POST!! Makes me really wonder if you are even telling the truth about working in a hospital, just because you are SO WRONG ABOUT EVERYTHING YOU SAID!! And that is PRETTY PATHETIC!!!!
Wow… You are the typical doc that has never experienced chronic pain or had a loved one that did. To say we should not live pain free is an arrogant statement and belittles your patients feelings and needs. While I agree Opioids should follow several other methods of pain control, you are being sadistic to say a patient should learn to live with pain and avoid a drug that can help them manage that pain. Even with Opioids or other pain meds/methods most of us STILL live in pain. In addition, MOST of us DO NOT want to be on any medication, but if the option is to be curled up in a ball versus taking a few pain meds a day to be functional… guess what I will choose. Maybe the medical field was not meant for you. Please do us all a favor and quit your profession.
All I know is that withdrawal from Tramadol OR it’s stronger counterpart, Tapentadol, is ABSOLUTE HELL. TOTALLY. Try something else. Outlaw this shit.
Interesting, I was on 200mg of tramadol a day for 2 years. Had chronic neck pain. It worked ok, often I had to supplement it with Advil. One day my PCP tells me it’s been upgraded to a schedule 1 narcotic and he can no longer prescribe it. I was like no problem it seems to not work that great any longer, maybe I’ve built up a tolerance whatever. I’m off the stuff basically cold turkey as I recall. No withdrawals. Nothing. Personally I cannot agree that it is anywhere near Percocet, Vicodin or even alcohol in the addictive/get you high department. It didn’t even constipate me like most opioids do. Never had problems driving on it at all. So sad to hear about people having their lives destroyed over a drug that I found to be very mild yet pretty effective for the most part…