How to examine, diagnose and treat non-traumatic eye complaints in an austere setting.
A 75-year-old man was seen during a field clinic at a refugee camp last year. He complained of blurred vision and a red eye that was originally painful, but that has lessened over a month. There was no history of known trauma and he denied any itchiness or discharge from the eye. The patient noted no prior medical or surgical history, but did have an old, traumatic enucleation of his left eye. He was not using any medications and not allergic to any medications.
On exam, he had no other abnormal systemic findings. Right pupil was equal, round, reactive to light and the extraocular muscles were intact. On visual acuity, he could count fingers and denied any diplopia.
- How would you describe this eye?

Fig 1a

fig 1b
- What physical exam steps can help you make a diagnosis?
- List five possible diagnoses.
- What is the treatment?
Description
The findings in Figure 1a show diffuse episcleritis and a 0.5cm white, round, inferolateral corneal defect with near complete circumferential white fluid layering.
The photographs in Figure 1b show 1.5cm white, vertical, inferior corneal defects. All three photographs are consistent with corneal ulcers — most likely caused by a previous foreign body.
Exam
For any eye complaint, a thorough history is crucial. Key questions include: length of symptoms, quality of pain, vision loss, discharge, trauma, toxic exposures, use of contact lenses and concern for a foreign body. [1]
On exam, it is important to first assess: visual acuity, pupil size, shape and reactivity to light and extra-ocular movements. Using a standard ophthalmoscope, a provider can look at the optic nerve and blood vessels. These two exam steps can be done in any setting efficiently without using a lot of time or resources. Visual acuity is a critical step and can be assessed with various simple methods, like reading a newspaper or pamphlet or using a pinhole device made from a paper cup can quickly assist in understanding a patient’s level of visual impairment.[2]
To completely evaluate the fundus, dilation eye drops are required and this is not practical in austere settings. However, the PanOptic (Welch Allyn) ophthalmoscope offers a 25% wider view of the fundus. There is an attachment piece called the iExaminer (see link below under Training Videos) that is useful for both rapid evaluation and potentially telemedicine purposes. A second similar, but smaller device is D-Eye. This is an attachment to the smart phone that allows for non-dilated fundal exams without a separate ophthalmoscope.
Topical anesthetic drops like Proparacaine followed by fluorescein staining and a Wood’s lamp (or the cobalt blue filter on a standard ophthalmoscope) are also useful to evaluate for corneal abrasions and ulcers. Corneal abrasions and ulcers are the most likely source of a painful, red eye.
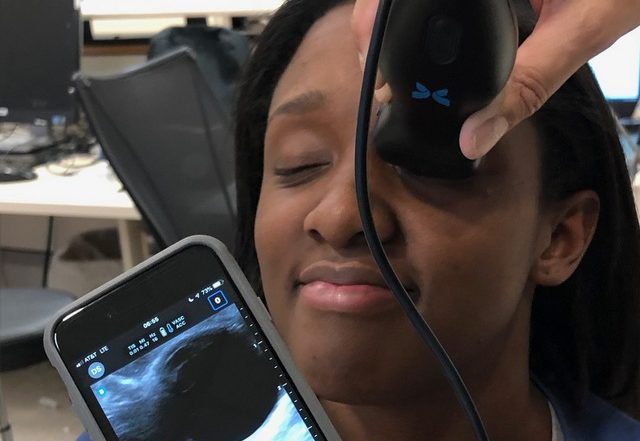
An even more in-depth evaluation could be done of the eyelids, eyelashes, lacrimal duct, anterior chamber, posterior chamber, lens, vitreous humor and intraocular pressure with a slit lamp exam (SLE). SLE is not available outside the clinic or hospital setting. Other exam options include: use of a Tonopen to measure intraocular pressures and ultrasound with a linear transducer probe to evaluate for retinal detachment (RD), posterior vitreous hemorrhage (PVH) and optic nerve sheath diameter (ONSD) — for glaucoma and intracranial hypertension. Tonopens are notoriously fickle for calibration and therefore hard to carry and keep in extreme conditions.
In brief, for eye trauma with significant contusions and/or edema, use of two cotton-tip applicator swabs or unfolded paper clips to retract the eyelids can help evaluate the globe. Ultrasound also has a role in determining presence of intraocular foreign body and traumatic globe rupture. Remember to bring or obtain ultrasound gel and wipes to clean the ultrasound transducer! Often times, given the credo of life, limb or eyesight, CT (computed tomography) and/or MR (magnetic resonance) imaging at a medical center with urgent surgical correction is indicated for such conditions.
Other Exam Considerations
Telemedicine capabilities for ocular exams are evolving and include both synchronous (live) and asynchronous (storage based) programs. Some concerns include: data security, image quality and legal issues such as patient privacy and malpractice.[3] As an affiliate of Johns Hopkins, our hospital uses a desktop-based telemedicine app. The patient is examined using a high-definition autofocus camera. The camera delivers real-time imaging to the ophthalmologist’s computer.
In addition, point-of-care, portable ultrasound devices can play a large role in ruling out critical eye processes such as globe rupture, foreign body, RD and PVH.[4] The main devices on the market are:
1) Clarius
2) Sonosite iViz
3) Lumify
4) Butterfly iQ
Apart from different interfaces, these four devices also have varying levels of clinical and education support. Clarius users can store images/data in the Clarius Cloud and access tutorials. Lumify has the most advanced program called Reacts that allows video conferencing, augmented reality and live chats. Sonosite offers extensive education via workshops, images and videos. Butterfly iQ (Figure 2) offers a storage Cloud, tutorials and a clinical images gallery.

As the role of telemedicine grows, particularly for ocular exams in low resource settings, such support features/apps will need to be refined to match the acuity of the patient being examined.
Differential Diagnosis
As seen in the case we have presented, foreign bodies can cause mechanical trauma to the surface of the eye, resulting in a corneal abrasion or ulceration. With any reports of antecedent injury or severe eye pain with foreign body sensation, a corneal defect should be considered. Removal of the foreign body using topical anesthesia, irrigation, and swab technique may be attempted, and all foreign body-associated corneal injuries should be treated empirically with broad-spectrum topical antibiotics.[5]
Current options include: Erythromycin 0.5% ointment, Trimethoprim-Polymyxin B 0.1% solution or Sulfacetamide 10% solution. For anti-Pseudomonal coverage, Ciprofloxacin 0.3%, Ofloxacin 0.3%, Tobramycin 0.3% or Gentamicin 0.3% solution can be prescribed. On our trips, the most cost-effective choice available in country is often Ciprofloxacin or Chloramphenicol. Most treatment courses are one to two drops to the affected eye, four times daily for three- to five-days.
Conjunctivitis (Figure 3) is a common condition that causes diffuse injection, possible mucoid or serous discharge, and itching or tenderness.

It is a clinical diagnosis that requires exclusion of more serious conditions such as keratitis (inflamed cornea), iritis (inflamed iris, also known as anterior uveitis) and angle closure glaucoma. Acute conjunctivitis can be generally classified as infectious (bacterial or viral) or noninfectious (allergic or mechanical/chemical insult). Depending on the suspected etiology, it can be treated with topical antibiotics, antihistamine/decongestants or lubricants.
A hypopyon (Figure 4) is a layered collection of leukocytes in the anterior chamber or bottom of the iris.

This is often accompanied by conjunctivitis and/or episcleritis. Untreated corneal ulcers are the most common precursor to hypopyon formation.[6] Viral infections, tuberculosis, drug reactions and HLA-B27 positive conditions are also known to form hypopyons. If the layered fluid collection has red blood cells, as seen in trauma, this is called a hyphema (Figure 5).

Arcus senilis, or corneal arcus (Figure 6), is a hazy, white, lipid-rich extracellular deposit in the peripheral corneal stroma.

It begins in the superior and inferior aspects and eventually spreads to encircle the entire circumference of the cornea. While considered a sign of hyperlipidemia and a potential increased risk for cardiovascular disease, this condition is a painless, benign condition present in 60% of individuals between the ages of 50 and 60 and in nearly 100% of individuals over 80 years old.
A cataract is the opacification of the intraocular crystalline lens (Figure 7), which gradually causes vision deterioration.[7]

The pathogenesis is primarily related to oxidative stress and protein accumulation, resulting in a painless, slowly progressive clouding of the normally transparent lens. While advanced age is the most common cause, other risk factors for cataract development include diabetes and smoking.
Pinguecula and pterygium (Figure 8 and 9) often arise as benign yellow-white conjunctival fibrous deposits. These are most often seen in tropical settings with significant UV light exposure.
- fig 8
- fig 9
Herpes simplex keratitis (HSK) can also be seen in austere settings (Figure 10). A classic dendritic pattern with fluorescein staining is seen with HSK.

Trachoma must also be considered when there is follicular, inflamed and injected conjunctiva with vision loss (Figure 11). It is caused by Chlamydia trachomatis and remains a leading cause of blindness around the world.

Treatment and Prognosis:
This patient had a chronic corneal ulcer with episcleritis and underlying arcus senilis. Given our limited diagnostic and treatment options, he was treated with the topical antibiotics we had available. Unfortunately, as is the case on most humanitarian outreach efforts, we were not able to follow-up on his outcome.
Summary:
Eye complaints are a common issue faced in humanitarian outreach missions. There are a number of conditions that can be rapidly diagnosed and treated.[8,9] Advancements in technological breakthroughs such as point-of-care ultrasound and telemedicine can aid in the evaluation, diagnosis and treatment of eye cases in austere settings.
Take Home Points for Non-traumatic Eye Cases:
- Quickly perform visual acuity, pupillary exam and check extraocular muscles
- If feasible, look at the fundus
- Point-of-care, portable ultrasound is fast, easy to do and can rule out several pathologies
- Treat suspected corneal abrasions and ulcers with available topical antibiotics
- For concerns over loss of vision and/or traumatic eye injuries, consider telemedicine and/or evaluation at a higher level of care
Things to Bring for Eye Exam:
- Pen light
- Ophthalmoscope (PanOptic preferred)
- Paper Clips
- Ultrasound (with gel)
References:
- Nickson, C. The Red Eye Challenge. Life in the Fastlane. Oct 2017.
- Iserson, K. Improvised Medicine. Chapter 30: Ophthalmology. 2016.
- AAO Telemedicine Task Force. Telemedicine for Ophthalmology Information Statement. Feb 2018.
- Landon, JD. The Butterfly Effect. https://epmonthly.wpengine.com/article/the-butterfly-effect/. Jan 2018.
- Wipperman JL, Dorsch, JN. Evaluation and Management of Corneal Abrasions. American Family Physician. 87(2): 114-120. Jan 2013.
- Turbert, D, Jimenez, E. https://www.aao.org/eye-health/diseases/corneal-ulcer-diagnosis. Nov 2018.
- Nartey A. The Pathophysiology of Cataract and Major Interventions to Retarding Its Progression: A Mini Review. Adv Ophthalmol Vis Syst 6(3): 178. Feb 2017.
- Paterson R, Drake B, Tabin G, Butler FK Jr, Cushing T. Wilderness Medical Society Practice Guidelines for Treatment of Eye Injuries and Illnesses in the Wilderness: 2014 Update. Wilderness Environ Med. 25 (Supplement 4): S19-29. Dec 2014.
- Lovas T, Butler F. Special Operations Forces Medical Handbook. Part 3: General Symptoms. Sections 3-22 to 3-29. June 2001.