For a generation of American physicians, the tragic and infamous case of Libby Zion evokes a multitude of feelings. Although the case is best remembered for the enduring effect it had on resident duty hours, for many of us it was the first time that we became familiar with the serotonin syndrome and the seemingly obscure drug interactions that can cause it.
A case that changed history and the elusive diagnosis at its core
For a generation of American physicians, the tragic and infamous case of Libby Zion evokes a multitude of feelings. Although the case is best remembered for the enduring effect it had on resident duty hours, for many of us it was the first time that we became familiar with the serotonin syndrome and the seemingly obscure drug interactions that can cause it. In this month’s EM:RAP, we take our listeners back to that fateful night at New York Hospital in 1984 and bring ourselves up to date with the latest understanding of the serotonin syndrome.
Libby Zion was an 18-year-old freshman at Bennington College in Vermont. In January of 1984, she had returned home to live with her parents in New York City as part of the college’s work-study program. Libby was recently under the care of a psychiatrist and had been prescribed phenelzine, a monoamine oxidase inhibitor, for depression. During this time she had also received other prescriptions, including imipramine, flurazepam, diazepam, tetracycline and doxycycline. In late February, she had a dental extraction for a carious tooth and Percodan (aspirin/oxycodone) was added to her growing list of medications.
On Thursday, March 1st, she began to suffer from what she believed to be a cold. She visited her pediatrician and was prescribed erythromycin and chlorpheniramine. On Friday, Libby left work early because she wasn’t feeling well. She was febrile and suffering from worsening “flu-like” symptoms. When her mother measured her temperature that Sunday afternoon, it was 102°F. The pediatrician was consulted by phone and he advised continuing the course of antibiotics. Her mother also began to apply an alcohol-based liniment. Apparently, Libby began to improve somewhat that evening – she appeared well enough for her parents to leave home for a party. At approximately 10 pm, however, Libby’s brother Adam called his parents to tell them that she had taken a turn for the worse. Upon their return home, they found her to have flushed skin, dilated pupils and roving eye movements. Sidney Zion, Libby’s father, called the family physician, who advised that she be brought to the emergency department.

Libby arrived at the emergency department at the New York Hospital at 11:30pm on March 4th. On her initial assessment she was noted to be writhing and agitated but able to convey her history. She was noted to be febrile to 103.5°F and also to have a right hyperemic tympanic membrane, a soft murmur and petechiae on her right thigh. A chest film was interpreted as normal and her hematology panel was notable for an elevated white blood cell count of 18,000/mm3. The resident in the emergency room administered intravenous fluids and obtained a set of blood cultures. After discussion with the referring physician, Libby was given acetaminophen and admitted to the hospital’s medical service at 2:00 am. She was then examined separately by both an intern and a resident, who made a provisional diagnosis of “viral syndrome with hysterical symptoms”. Additional cultures were ordered, antibiotics and phenelzine were withheld and she was prescribed meperidine for agitation and shivering. At 3:30am, Libby received an intramuscular injection of 25mg of meperidine. Between 3:30am and 4:30am, her agitation increased, she was noted to be confused and she began to thrash around in bed. Physical restraints, in addition to 1mg of haloperidol, were administered and finally she began to settle. The restraints were removed and she was able to take her next acetaminophen dose by mouth. Unfortunately, her agitation returned shortly thereafter and her temperature began to climb even higher. It was last recorded at 107°F. Despite cooling measures, including a cooling blanket and cold compresses, she deteriorated, finally suffering a respiratory and cardiac arrest at 6:30am from which she could not be revived.
Most discussions of this infamous case center around the level of supervision and long work hours of the resident physicians involved. But the truth is that even after her death and with the benefit of hindsight, the senior physicians involved in the case did not appreciate what errors were made. In fact, two days after her death, the medical examiner listed the preliminary cause of Libby’s death to be bilateral bronchopneumonia. In over a decade of legal proceedings that followed, it became apparent that most physicians were unaware of serotonin toxicity and of the potentially fatal interaction of meperidine and monoamine oxidase inhibitors.
According to Dr. Sean Nordt, EM:RAP’s resident toxicologist, serotonin toxicity is a more accurate term than serotonin syndrome. That is because in contrast to neuroleptic malignant syndrome, which is a rare, idiosyncratic reaction to haloperidol and other antipsychotic medications, serotonin syndrome is a predictable consequence of excess serotonin. This excess is a result of overdose or of a combination of drugs with serotonergic activity. The clinical picture of serotonin toxicity can best be described as a triad of cognitive, autonomic and somatic effects. In mild cases, the cognitive effects may simply consist of abnormal mood, such as hypomania, but in severe cases, mental status is altered and patients may experience severe agitation and hallucinations. The autonomic effects consist of diaphoresis, hypertension, hyperthermia, tachycardia and diarrhea. In severe cases, marked hyperthermia can give rise to additional complications, such as rhabdomyolysis, seizures, metabolic acidosis and disseminated intravascular coagulation. Finally, the somatic effects are essential for the diagnosis; these are myoclonus, tremor and hyperreflexia with clonus.
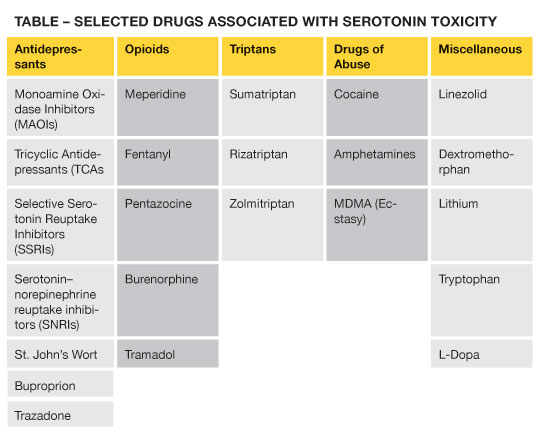
Although serotonin toxicity is predictable to a certain extent, estimating the risk of a clinically severe syndrome in individual patients is difficult. For example, fatalities in patients taking a single serotonin reuptake inhibitor (SSRI), even in very large doses, are distinctly rare. Severe toxicity appears to be associated with combinations of agents that act through different mechanisms. Many of the severe cases arise when an antidepressant is combined with over-the-counter medications such as dextromethorphan and/or sympathomimetic drugs of abuse, such as cocaine and MDMA (ecstasy). In fact, although Libby Zion denied cocaine use, post-mortem tests revealed cocaine metabolites in several of her tissues. The accompanying table lists drugs most frequently associated with serotonin toxicity.
The differential diagnosis of patients with altered mental status and fever is broad, and includes central nervous system structural lesions, infectious causes such as meningoencephalitis, thyroid storm and non-convulsive status epilepticus. The toxicologic differential includes sympathomimetic overdose, sedative-hypnotic withdrawal, salicylism, malignant hyperthermia and anticholinergic toxicity. The one diagnosis most frequently confused with serotonin toxicity is neuroleptic malignant syndrome. Distinguishing between the two can be especially difficult in patients who are exposed to multiple agents that are implicated in both syndromes. Neuroleptic ma
lignant syndrome, which results from dopamine blockade, tends to present more gradually than serotonin toxicity. More importantly, in neuroleptic malignant syndrome movements are decreased (bradykinesia), and there is lead-pipe rigidity of the extremities, whereas with serotonin toxicity movements are increased (hyperkinesia) and clonus is present.
There is no laboratory test to confirm the diagnosis of serotonin toxicity. If the diagnosis is being entertained, all medications that may be contributory should be immediately discontinued. Supportive care, tailored to the severity of the patient’s symptoms, is the mainstay of therapy. Benzodiazepines are used for agitation and muscular hyperactivity, and in the most severe cases, paralysis with non-depolarizing agents such as vecuronium may be necessary to stop the cycle of muscular contraction and its sequelae. Antipyretics are not indicated, as the hyperthermia is not mediated by the hypothalamus but rather by the muscular hyperactivity itself. Cyproheptadine, a serotonin antagonist, is recommended by most experts as an adjunctive treatment to supportive care, although data to support its use is based only in theory and a limited number of case reports.
Dr. Swadron is the vice-chair for education in the department of emergency medicine at the LA County/USC Medical Center. He is an associate professor of clinical emergency medicine at the Keck School of Medicine. EM:RAP (emergency medicine: reviews and perspectives) is a monthly audio program that can be found at www.EMRAP.org



6 Comments
She very well was in SS before she arrived at the hospital. The first mistake of many was the pediatrician giving her chlorpheniramine (the over the counter antihistamine) As Arvid Carlson showed decades ago, chlorpheniramine is an inhibitor of serotonin reuptake. To put into perspective, the Ki for SERT (serotonin xperoter) for chlorpheniramine is roughly the same as for the SSRI fluvoxamine (Luvox) or Norfluoxetine (the primary metabolite of Prozac)
Exactly, she arrived to the ER with serotonin syndrome, also potentially triggered with cocaine. So they made 2 mistakes: Not recognizing the syndrome since the beginning and adding more gas to the fire with the meperidine.
would a drug screen have helped?
intubation with cooling blankets ? till labs arrived?
Physicians are still not paying attention to this potential problem when prescribing medications. Polypharmacy makes Serotonin Toxicity a living and breathing problem.
I suffered from Serotonin toxicity after having total hip replacement surgery. I was taking 150mg of Zoloft daily before surgery. I thought I just had restless legs and vomiting from the pain meds. My sister saved my life by getting me to the ER. I ended up ripping catheter, IVs and anything else connected to me and tried to get up. I kicked a nurse in the head and ended up restrained, ankles and wrists. Thank God I don’t remember it. I got out three days later. Scary!!!
Hi I might think my mother may have this serotonin syndrome. Not sure if this is allowed but is there anyway you could get a hold of me to discuss symptoms. Me and my family are lost on what to do and the doctors have been no help. We have travels to a bigger city to see if we can get better treatment. Text 307-433-4333