Not a Dollar Store Diagnosis
“Ugh, what a waste of time and resources…” you hear your intern mutter under his breath. You decide not to let a good mentoring and teaching moment slip past you, so you reply, “What’s going on? What can I do to help you?” Your intern looks so exasperated with the patient that he just saw that he doesn’t even register your look of consternation.
“I’m so sick of patients coming into the ED and using us as an urgent care clinic or primary care office.” He sulks his way to his computer so he can start typing his note. “I’ve just spent the first half of my shift taking care of patients with symptoms that they could have treated with simple over-the-counter medications, and now I have another patient who should have gone to the dollar store and peed on a pregnancy stick before she checked in to be seen.”
The senior residents in the doc box with you overhear the conversation and feel compelled to chime in with their own various opinions. You catch snippets that range from “Yeah, it’s ridiculous what we are asked to see” to “Don’t be such a jerk! Maybe they have no other place to turn” and “Do you want to eat an empathy sandwich before you see any more patients today?”
You let them vent, commiserate, and self-regulate for a bit before you speak up and offer, “Why don’t you tell me about that lady you just saw in room nine? Maybe we can open up that room for another patient if she really doesn’t have anything that requires emergent attention today.”
Happy to escape the taunting, your intern asks you to walk over to the ultrasound machine so he can pull up and show you some images while he is telling you about the patient. The lady he just saw is a 33 year-old G4P3003 who comes into the ED with mild abdominal pain and vaginal spotting. She missed her last period and told the nurses at triage that she wants to know if she is pregnant. She has had some mild abdominal cramping and noted a few “drops” of blood on her underwear.

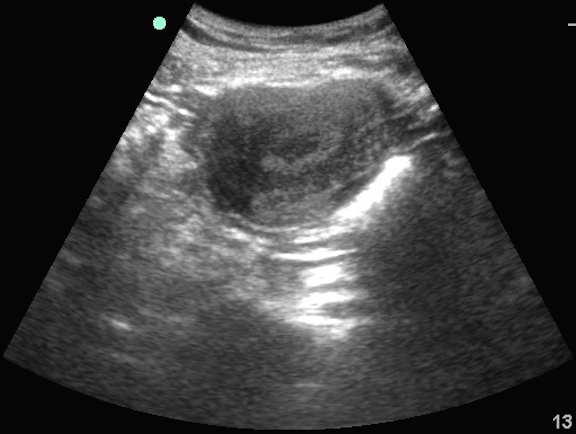
1. Transabdominal pelvic ultrasound (transverse view)
Her vital signs include a BP of 100/66 mmHg, HR 80 bpm, RR 16, O2 sat of 100% on RA and temperature of 37.3°C. On exam, your intern noted some mild suprapubic tenderness to palpation and he reports that her pelvic exam showed some scant blood in the vaginal vault, a normal cervix, closed cervical os, no abnormal discharge, and no adnexal fullness or tenderness. He goes on to tell you that a CBC, type and Rh, quantitative serum beta-hCG level, and urinalysis were sent from triage and that they were all “as expected.” She’s pregnant with mild anemia and has a quantitative hCG level of 17,680 mIU/mL. Her labs, urinalysis, and pelvic exam results were otherwise unremarkable.
As your intern wraps up his presentation, he pulls up the transabdominal pelvic ultrasound images he obtained on her, and says “I told her she’s pregnant, reviewed her results with her, and advised her to follow up with her OB as an outpatient.”

2. Transabdominal pelvic ultrasound (saggital view)
You review her ultrasound images. What do you see? Should you go along with your intern’s plan? Scroll down for conclusion.
You carefully scroll through all of the images your intern obtained on his transabdominal ultrasound and pause dramatically and furrow your brows for effect. You carefully point out to your intern that the gestational sac you see on image 2 doesn’t appear to be situated in the endometrium where you would expect in a normal pregnancy. On ultrasound, you would hope to see the gestational sac implanted and growing in the endometrium up closer to the uterine fundus. The patient’s gestational sac appears to be really low and anterior in the lower uterine segment (Image 3).

3. A normal gestational sac visualized in the endometrium near the uterine fundus in the image on the left. The patient’s gestational sac is in the anterior lower uterine segment in the image on the right.
On further review of the images, you are actually concerned that there is very little myometrium between the gestational sac and the abdominal wall. Could this be a cervical ectopic pregnancy? Or an ectopic pregnancy implanted in her old Caesarean scar? If she was having a miscarriage, you would still expect to see the gestational sac surrounded by more endometrium and myometrium. This is really a much more complicated case than anticipated.
As you are thinking and teaching out loud, you notice that your team of residents in the doc box have gathered around to see what the cool teaching case is all about. You walk them through what the ultrasound shows and teach them about the rare diagnosis of a Caesarean scar ectopic otherwise known as an intramural ectopic. Topping off your teaching points, you enlighten them about inpatient treatment options with local injections of methotrexate under radiographic guidance, and the theory that blastocysts can migrate through dehiscent tracks from the endometrium into the myometrium after trauma, previous surgeries, manual placental removal, placenta accreta, or in vitro fertilization attempts. On further review, the patient has had 3 previous Caesarean sections and had placenta accreta with her last pregnancy.
The OB consult team opts to admit the patient and wants to obtain an MRI of her pelvis to try help differentiate between a cervical ectopic versus an intramural ectopic. As your intern rips up the discharge paperwork, you see your senior resident flash the winningest of smiles and jests “Guess that one’s not a dollar store diagnosis, is it?”
Pearls & Pitfalls in Evaluating a Caesarean Ectopic Pregnancy on Ultrasound
- Use point of care ultrasound to obtain valuable information about your patients quickly at the bedside.
- Always begin your pelvic ultrasound with a full bladder and a transabdominal scan to map out the important organs and structures. A full bladder provides an excellent acoustic window.
- On your transabdominal scan, determine how the uterus is lying anatomically and determine if there is any obvious free fluid, large adnexal masses, or intrauterine findings. Identify the uterine fundus, endometrial stripe, and region where you expect to see the cervix.
- Scan systematically through the uterus in both a transverse and sagittal plane.
- If you think your patient is pregnant and you see a gestational sac, pay close attention to where the gestational sac is situated in the uterus. In a normal pregnancy, the gestational sac will be seen as a hyperechoic ring surrounding an anechoic collection of fluid. This sac should be embedded in the endometrium closer to the uterus fundus than the cervix.
- If you see a gestational sac that is sitting in the lower, inferior portion of the uterus and closer to the cervix, think about potential diagnoses such as an intramural ectopic pregnancy, an ectopic pregnancy in the cervix, or miscarriage in process.
- Although intramural ectopic pregnancies are very rare, they are very important to diagnose because of their risk for myometrial rupture and life-threatening hemorrhage.
- If the point-of-care transabdominal ultrasound demonstrates an abnormal location of the pregnancy, a transvaginal ultrasound is required for better visualization of the position of the intrauterine pregnancy. The patient may require further evaluation with an MRI or 3-dimensional transvaginal ultrasound imaging after OB consultation.
- The best way to minimize errors is through experience, so scan lots of normal anatomy. The more scans you do, the better you will be able to differentiate abnormal from normal, even when you may not be sure exactly what the abnormality is.



1 Comment
I’m a sonographer – I diagnosed a C-section ectopic a few years ago at a clinic. The patient was sent to the big-name tertiary hospital 30 miles away. They diagnosed it as a normal IUP. Four days later, my diagnosis was surgically dx’d to be the correct one. At least she made it to surgery and survived to look after her other 4 kids.