A look at the psychiatric medical screening exam (PMSE), and the age-old misconceptions that too often pit one specialty against another.
Nothing seems to illicit suicidal ideations in me more then arguing with a psychiatrist or mental health nurse that a patient I have evaluated and cleared for psychiatric evaluation does not need a battery of tests prior to transfer.
A look at the psychiatric medical screening exam (PMSE), and the age-old misconceptions that too often pit one specialty against another.
Nothing seems to illicit suicidal ideations in me more then arguing with a psychiatrist or mental health nurse that a patient I have evaluated and cleared for psychiatric evaluation does not need a battery of tests prior to transfer. This disagreement usually takes place at 2 AM during a very busy shift. To add to the madness, the patient usually presents first to the psychiatric facility with the complaint that they are suicidal and are thinking of jumping in front of a bus only to be told to “go to the emergency room first to get a medical clearance exam”. And then the patient arrives to the ED by bus!
This article will look at the history and evolution of the emergency department medical clearance exam for psychiatric patients, the misconceptions that have developed regarding this process that too often pit two specialties against one another. We’ll evaluate the data to determine what should routinely be included in the clearance exam, and identify solutions that will simultaneously satisfy both specialties in order to expedite the emergency psychiatric evaluation these patients are requesting. Throughout this article I will refer to the medical clearance exam as the psychiatric medical screening exam (PMSE) since the term “clearance” is a misnomer in this situation and has generated unrealistic expectations of this screening exam.
 More than 62 million Americans (22.2%) have some form of mental disorder. Of this group, 8.7% have what is categorized as severe mental illness. Ninety percent of Americans with severe mental illness are unemployed and 50% do not receive psychiatric treatment. When you add EMTALA to the above statistics it is not a surprise that 6 to 12% of all US ED visits are related to psychiatric complaints and, to make matters worse, the average ED length of stay is double that of non-psych patients (median 5.5 hours) exacerbating ED overcrowding. Unfortunately, most EDs do not have the expertise or resources to provide these patients with a proper emergency psychiatric evaluation and so these patients most often require a transfer to a psychiatric facility. This is usually where the friction begins. Although it can be agreed by both specialties that psychiatric illness can coexist with medical illness, can exacerbate medical illness, can be a presenting symptom of a medical illness, and can coexist with substance abuse emergencies, no consensus has been reached regarding a standardized clinical pathway outlining the scope and extent of the PMSE. The need for mandatory ancillary testing appears to be the greatest barrier to this consensus. It seems ironic that psychiatry relies on emergency medicine to perform the PMSE because they lack the expertise, yet they mandate what needs to be included in the screening and have the final say of when the screening is complete (usually over the phone without ever seeing the patient).
More than 62 million Americans (22.2%) have some form of mental disorder. Of this group, 8.7% have what is categorized as severe mental illness. Ninety percent of Americans with severe mental illness are unemployed and 50% do not receive psychiatric treatment. When you add EMTALA to the above statistics it is not a surprise that 6 to 12% of all US ED visits are related to psychiatric complaints and, to make matters worse, the average ED length of stay is double that of non-psych patients (median 5.5 hours) exacerbating ED overcrowding. Unfortunately, most EDs do not have the expertise or resources to provide these patients with a proper emergency psychiatric evaluation and so these patients most often require a transfer to a psychiatric facility. This is usually where the friction begins. Although it can be agreed by both specialties that psychiatric illness can coexist with medical illness, can exacerbate medical illness, can be a presenting symptom of a medical illness, and can coexist with substance abuse emergencies, no consensus has been reached regarding a standardized clinical pathway outlining the scope and extent of the PMSE. The need for mandatory ancillary testing appears to be the greatest barrier to this consensus. It seems ironic that psychiatry relies on emergency medicine to perform the PMSE because they lack the expertise, yet they mandate what needs to be included in the screening and have the final say of when the screening is complete (usually over the phone without ever seeing the patient).
At the University Medical Center of Southern Nevada (UMC) we performed a survey of emergency physicians to identify practices and requirements regarding the PMSE. We found that mandatory laboratory testing regardless of patient’s history and physical exam occurs in EDs throughout the nation and found that 84% of the time these mandatory tests are required by the psychiatric facility even though the EP does not feel they are required. How has this occurred? Is this any different then a neurosurgeon refusing to take a patient with a large subdural hematoma to the operating room until the patient’s alcohol level comes back?
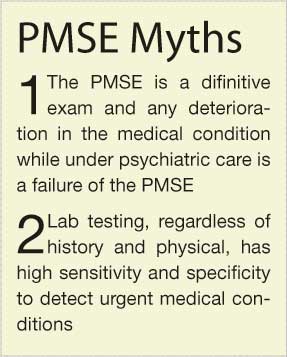
Two major misconceptions psychiatrists have regarding the PMSE has led to this situation. The first misconception is that the PMSE is a definitive exam and that any exacerbation or deterioration of a patient’s medical condition while under psychiatric care is a failure of the PMSE rather than the natural progression of a patient’s condition. This misconception places unrealistic value on the PMSE. I can guarantee that any discussion you have with a psychiatrist regarding mandatory ancillary testing will always come back to an anecdotal case the psychiatrist had of a patient “medically cleared” who turned out to have a brain tumor. They will then use this as the reason why the PMSE must include extensive testing on all patients while failing to understand that a better history and physical exam by the EP would be the correct mandate since a mandatory CBC and chemistry panel does not help diagnose a brain tumor.
This leads to the second misconception, that laboratory testing, regardless of history and physical exam, has high sensitivity and specificity to detect urgent medical conditions. Psychiatrists will cite past studies that indicate 63% of patients with psychiatric symptoms were found to have an organic etiology of their presentation, yet fail to realize that these studies looked at all comers, and that many of these patients would fall into the category of altered mental status or delirium by EPs and would not be considered patients applicable for a PMSE. Past studies also suggest that routine laboratory testing alone had a sensitivity of 20% in detecting medical illness. The fact that the sensitivity is anything other than 0% is data enough for psychiatry to require mandatory laboratory testing even though medical illness was not defined. This low sensitivity is viewed by most EPs as proof enough against this practice mandate.
We presented a study at the Society of Academic Emergency Medicine annul meeting titled “Mandatory laboratory testing for emergency department psychiatric medical screening exam: Useful or useless?” This was a retrospective chart review of 1095 consecutive psychiatric patients presenting to the ED for medical clearance. Mandatory laboratory testing included CBC, Chemistry 7, alcohol and toxicological serum testing totaling 8872 laboratory tests. Records were analyzed to determine if the results of mandatory laboratory testing had any effect on patient management or disposition. Fifty-four [4.9% (54/1095)] patients were considered to have moderate to severe abnormalities, a complete database was obtained for 29 [54% (29/54)] of these patients. Mandatory lab testing identified 12 [41%(12/29)] patients in which history and physical exam would not have predicted these results and of these patients 6 had no management changes and 6 had minor management changes. From this study, it may be concluded that mandatory laboratory testing in the psychiatric medical screening exam of psychiatric patients presenting to the ED rarely yields abnormalities that would not have been predicted based on the history and physical exam alone or resulted in a significant management change. This practice is also extremely expensive, subjects the health care workers to unnecessary exposure risks and is time consuming for the staff and patients.
Before all you EPs pick up pitchforks and storm your local psychiatric facility, realize we also have been part of the problem. Past studies have indicated that the PMSE was not well documented and perhaps not well preformed by EPs. Past chart review studies revealed many common documentation deficiencies, including lack of vital signs, mental status exam, and most frequent and concerning lack of a complete neurological examination. Failure to provide a complete PMSE results in inappropriate patients being sent to psychiatric facilities and becomes
ammunition for psychiatry to mandate the scope and extent of the PMSE. It is the responsibility of the EP to provide an adequate PMSE, which includes: thorough history, complete physical exam, diagnostic tests if indicated based on the history and physical exam. The EP must also consider a more extensive screening on patients with the following: abnormal vital signs, histories suggestive of medical illness, physical exam abnormalities, preexisting/new medical complaints, elderly, substance abuse, and patients with no prior psychiatric history.
Urine toxicology and alcohol testing as part of the PMSE continues to be debated. The data indicates that in a patient who is awake, alert, and cooperative, routine testing does not affect ED management. However, it may be requested by the psychiatric facility since dual diagnoses may affect the psychiatric management plan. However if performed, then the pending results should not delay psychiatric evaluation or transfer. As for the blood alcohol level, there is no recognized level to suggest when psychiatric evaluation can begin. Commonly the legal limit to drive a car has been the level of choice, but does not equal decision-making capacity (DMC). Psychiatric assessment should begin based on patient’s cognitive ability rather than a specific alcohol level.
The best solution to improving and expediting the care of these patients presenting to the ED with psychiatric complaints is open and regular communication with the psychiatrist and psychiatric facilities that will ultimately be caring for your patients. Establishing a committee made up of representatives from the local EDs and psychiatric facilities that meets on a regular basis to discuss process issues, policy and procedure, and to review cases that may offer performance improvement information would be much more beneficial then ordering thousands of ancillary tests that do not appear to offer any benefit.
Additional References
Sood TR, McStay CM; Evaluation of the psychiatric patient; Emerg Med Clin N Am 2009; 27(4): 669-683.
Hillard R, Zitek B; Emergency psychiatry. McGraw-Hill 2004.
J.D. McCourt, MD, FACEP
Medical Director Adult Emergency Department University Medical Center of Southern Nevada
Assistant Professor, Department of Emergency Medicine, University of Nevada School of Medicine