First let’s looks this 17% of GDP figure. Perhaps you’re thinking that this seems like an appropriate amount for a prosperous nation to spend on its health care. Wrong. No matter how good it is, health care will always be a supportive service, not an economic engine, which means we must always keep this massive expenditure in check. You can’t spend all of your money on health care because then nothing is actually generating anything. You need to have a product that you either build or sell or invent.
Some people counter that those health care dollars are mostly spend domestically. But the point is, it’s spent, and then I as an individual don’t get to spend it and its productive capacity has been lost. The Singaporese spend about 5% of their GDP on health care and have greater longevity and better infant mortality. If we had that expenditure we would actually have a budget surplus. We could pay against the debt.
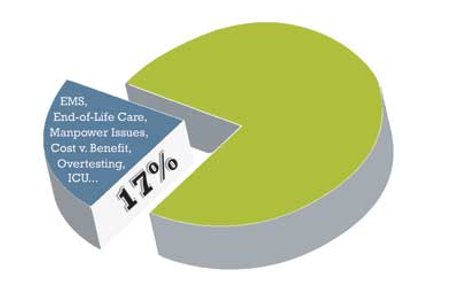
The next issue is the pooled money. If health care is going to operate largely out of pooled resources, we must get a handle on how our money is being spent, and where it’s falling through the cracks. Below I’m going to talk about nine ways that we could save millions in health care, in areas that no one wants to touch.
As a so-called necessary health care expenditure, I think EMS is the largest hoax ever foisted on the American people. There is no data, not one study, which shows that anything beyond the intermediate level – basic EMT with defibrillator capabilities – does anything in the long run to change the health care of the United States. The problem is this: it’s a hidden cost. Do you realize what it costs for a fire department to simply keep everyone current with their ACLS cards? This is what Casey Stengel would call a long run for a short slide. This has become a local government power base and the numbers aren’t even figured in to the overall health care costs in the United States.
Let’s look at the Germans. They’ve made decisions. They have a board which asks the question: Does this new therapy really work? They are not run by drug company advertising first with the larger interest of society second. And if the national board of medicine in Germany doesn’t say that a procedure is available, you can’t get it in Germany. The best example is a bone marrow transplant in stage two breast cancer. It doesn’t work, and it’s not available in Germany. They say it’s no different than flipping a coin. In California there was an insurance company sued for $17 million for not offering that therapy. You cannot litigate your way to success. No country ever sued its way to greatness.
There comes a time to die. Why would you have people without intellectual function on long-term ventilators? It’s crazy. Several people have placed a dollar value on restrictions to end-of-life care. I will claim that it is ten times the cost of all emergency care in the United States. Furthermore, I think this expense could be reduced by 50% with more responsible end-of-life decision making.
Doctors used to be people who had sort of a mechanical bent. They figured things out. Now they’re a bunch of intellectuals who send off a bunch of numbers and hope that an answer falls out. You don’t need a test in every situation. And, a lot of our tests don’t answer the question on the table. And all it does is feed the plaintiff’s attorneys who say, “Well you didn’t get this!” See I don’t think that the majority of kids hit on the head need a CT scan. I have the lowest rate of the use of CT in our department for head injury and headache. By far. Why? Because I know how to examine. We need to return to a cost-benefit analysis and ask the question: What is the reasonable miss rate. We’ve decided in this country that the number is zero, so you don’t get sued. I believe that through more intelligent testing we could save at least 10% on the health care dollar.
You hear all of these nit-wits complain about their Press-Gainey scores; I have good Press-Gainey scores. I can convince a patient of anything. I say, “If it was me…”, or, “If it was my child, this is what I would do.” If you do it that way, if you truly empathize and communicate clearly, your Press-Gainey scores will be just fine.
The average emergency physician spends between 12 and 15 times their annual salary on testing. That number has been looked at several times. As soon as you order that CT on a basic headache, what have you done to that visit? The EP got something like $68 for seeing the patient. Now there’s $1000 that just went down the drain on a patient whose odds of having it be a benefit are small. Not to mention the fact that the federal government this year will spend more money on EKG overreads than it does on emergency department visits.
Change happens all the time, but progress doesn’t happen very often. For example, Nesiritide came out for congestive heart failure. It was a disaster. They spent $7 million the first week it came out in journal advertising. Now, look what’s happening with Vytorin. You talk about a drug that has now decided to head south on the last train to hell. We need to sit back a little bit and not jump on the bandwagon of every two-bit piece of crap coming out.
I review for five journals. Our journals tend to only print positive results. We never print negative results. Here’s something that needs to be done in this country. We need to have a registry of studies so that everything that is eventually going to be published has been registered. That way, if there’s a negative trial and it’s withdrawn, you have to account for that one too. The problem is that we don’t even know what we don’t know. You can always cherry pick a study to give you what you want. That’s not science.
Marginal benefit isn’t the exception these days in health care, it’s the norm. When I started in medicine in the late 60s, about 3.5 percent of the health care dollar was spent on medications. That number is now 20%. And what we’re buying for the dollar is extremely poor. And that’s at all ends of the spectrum. If you go to Holland today your children with otitis media will not get an antibiotic during the first three days. Those kids are going to be able to cure themselves. In this country, no parent thinks they have been treated unless they leave with a bottle of pink stuff that smells like bubble gum. What we should do is just give them a bottle of bubble gum and let them leave!
Europeans basically run their health care system as a federal HMO. I was a visiting professor at Cambridge and experienced the British system first hand. Britain has a global budget for health care which it has to function within, making rank order decisions. Every financial system has a governor that controls its flow and output. In the free market, people control it by having to pay the price of what they want. You have to take the money out of your pocket. When people don’t see the money they do not understand what the hell’s going on. There was a time in this country when doctors knew people were paying the bill and they’d say things like, “I think there’s a cheaper way we can do this.” Sorry, the good old days are gone. In essentially no medical schools or training programs is cost effectiveness even discussed any more.
Another place where we could save millions is our use of the ICU. I’ve never understood no codes or DNRs in ICUs. What are we doing? This should be where we apply high level technology to people who have a reasonable chance of making it. You’re looking at 8-10 percent of hospital costs are going into their ICUs. In fact, at certain kinds of hospitals, it could be up to 15%.
The big money savings are in workforce: who is doing what tasks, and for how much. In case someone hasn’t looked recently, there’s a nursing crisis in the United States. Nurses should be doing nursing functions. That is, the monitoring of critically ill patients. Emergency department techs can do the majority of the other work. 90% of what has to be done in the ED is hand work, not head work. I don’t think an RN should ever be bringing a patient back to the room, getting them undressed or pushing them to X-ray.
Furthermore, I think there needs to be a progression of jobs. It would be great if we could take EMTs, not overtrain them, and then after five years or so, transition them into in-hospital techs. When you think about it, EMTs is a young person’s job. You don’t want to be cutting people out of cars at age 60. I can barely get in my car at age 60!
Finally, Most routine care situations don’t need a doctor. The best example is pediatrics. We’re one vaccination away from wondering why we even train pediatricians at all. Most of that care is book-keeping. Did you show up? How are you progressing? And then, knowing when to do intervention on real problems. And, there’s certainly all kinds of care being given out at nursing home type facilities which we need a different kind of provider for.
What do we think the society owes the individual, and what does the individual owe the society? I think that the individual owes the society something which no one wants to talk about, and that is a time to die. At a certain point in time, you can’t afford to do everything for everybody. No western democracy has succeeded in its health plan without grappling with this most basic of questions.
The silver lining to all of this doom and gloom? Take pride in the fact that you, an emergency physician, occupy perhaps 1.8 to 2.2 of the health care dollar of the United States, and it’s the best 2.2% this country ever got. When you look at it, we’re useful!
Greg Henry, MD, is the founder and CEO of Medical Practice Risk Assessment, Inc. Dr. Henry is a past president of ACEP and directed an emergency department for 21 years. Dr. Henry has had an interest in economic issues for over 30 years.