When Broadway composer Jonathan Larson collapsed the night before the opening of his magnum opus, Rent, it set in motion a series of errors and unfortunate ED encounters. The result was a multi-million dollar lawsuit and many lessons learned the hard way.
An Excerpt from Chapter 4 of Bouncebacks! Medical and Legal
When Broadway composer Jonathan Larson collapsed the night before the opening of his magnum opus, Rent, it set in motion a series of errors and unfortunate ED encounters. The result was a multi-million dollar lawsuit and many lessons learned the hard way.
An Excerpt from Chapter 4 of Bouncebacks! Medical and Legal
The Patient’s Story
At the age of 22 Jonathan moves to New York City to pursue his dream of writing a musical. Like most struggling artists, life isn’t easy. He spends weekends waiting tables at the Moondance Diner in Soho. He spends weekdays at his keyboard writing songs. His tattered four-story walk up is so tiny, there is a bathtub in the kitchen. Through the years, he has some success writing for Sesame Street and cabarets, but not the big break he has been hoping for. In the late 80’s, he begins work on a new project; he has a vision to create a modern version of “La Boheme.” He doesn’t merely want to update the opera, but to transform the American musical tradition, appealing to a younger audience raised on MTV, modern film, and changing social values. After two years of hard work, the project is suspended, but he returns to it with a passion after three young friends die of AIDS.
Finally, in 1994, he receives a grant to develop his musical at The New York Theater Workshop. He sends his dad a note: “Dear Dad, I quit work. Love, Jon.” In December 1995, dress rehearsals begin. One month later, on Sunday January 21st , he is in the theater for the final week of rehearsals, visualizing his last seven years of hard work. After dinner, at 6:30 to be exact, he is suddenly struck by intense chest pains. He is short of breath and dizzy. He tells a friend, “You’d better call 911, I think I’m having a heart attack,” then falls to the floor between the theater’s last two rows.
An ambulance rushes him to Cabrini Medical Center. On the way, the paramedics record their diagnosis: “Pleuritic chest pain.”
The Doctor’s Version

Date: Sunday January 21, 1996 at 18:45
Place: Cabrini Medical Center, New York City
Chief complaint (per nurse at 18:45): Inspiratory chest pain. Rates pain as 7/10
Chief complaint (per physician at 19:00): Epigastric abd. pain
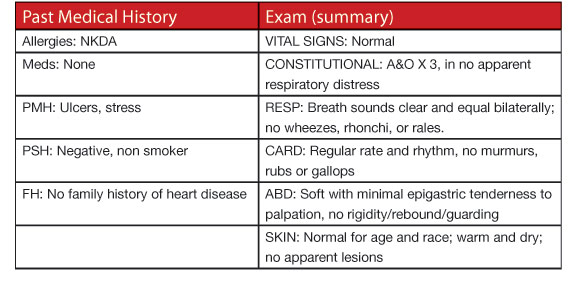
History of Present Illness (19:00): Pt. states he ate a turkey sandwich, which didn’t taste right. Had dinner and smoked marijuana prior to developing Sx. Hx of ulcers but no hx cardiac disease, no smoking or cardiac risk factors … just finished producing a play… increased stress: Review of systems negative for nausea, vomiting, or diarrhea.
ED Course
• Dizzy spell while in the radiology department. Nursing documentation records breathing
problems and dizziness while in the ED including the patient saying, “I can’t take a
breath.” It is unclear from records whether the doctor was informed of this episode.
• “He was pale and clammy,” says best friend Jonathan Burkhart, who met him at the hospital.
“You’ve never seen a person breathe as hard as he was breathing.”
• Jonathan’s friend asks the doctor for an update and is told, “I can’t find anything wrong.
You’ll be out of here in one hour since I want to pump his stomach.’’
Risk management/patient safety issue #1:
Error: Not reading or acknowledging the nurse’s notes.
Discussion: We have all had the medical school experience of presenting a patient’s history only to find the attending gets a different history, usually with you feeling nine inches tall. Just because a nurse records a history does not mean the patient needs thousands of dollars of tests: “the worst headache of his life,” “child turned blue,” “pleuritic chest pain.” But it does mean the documentation needs to be acknowledged and either confirmed or refuted by the physician. The options include:
1. Record that you have read the nurse’s note and have discussed it with the patient (and/or family), and they deny saying the documented phrase. I usually note that I have confirmed this twice. Two doctors beat one nurse, even if it’s just the same doctor asking twice.
2. Seek other ways to confirm which party is getting the most accurate information, such as family members or a squad report. (Note: realize patients may change their story, such as an adolescent who told the triage nurse he was suicidal, but denies it to you since he now realizes he will be “pink slipped”).
3. Speak with the nurse to confirm the history documented is actually the history received. Just as speaking with the nurse is important, valuable information can be discovered from the paramedics. Their observations are particularly valuable in seizure patients, motor vehicle accidents (“When we got there he was completely alert”) and with alteredconsciousness elderly patients (“Doc, we run on this guy every week, and he is always non-verbal.”) In this case, the paramedics found a patient complaining of inspiratory chest pain who had just had a syncopal episode—not a story easily swallowed as food poisoning.
Teaching point: Ignore the nurse’s documentation at both your patient’s and your own peril.
Risk management/patient safety issue #2:
Error: Not digging deeper.
Discussion: A patient with food poisoning would be expected to have more symptoms than mere epigastric abdominal pain (i.e., vomiting or diarrhea). These associated symptoms are not essential for the diagnosis, but without them an alternative explanation should be considered. Was anyone else who had the turkey sandwiches sick? Is there any dizziness or sweating, or at least some nausea? Are there other symptoms (chest pain) which would lead the physician to an alternate diagnosis?
Teaching point: When the story is not consistent, return to the bedside and:
1. Confirm the history.
2. Inquire about other important symptoms based on ddx of “can’t miss” diagnoses.
3. Re-examine the patient.
4. Ensure disease process is not progressing.
5. Record a progress note.
Risk management/patient safety issue #3:
Error: Performing bizarre therapy.
Discussion: We barely pump stomachs for drug overdose anymore; it is hard to see how it would be helpful to remove a “food-poisoning” toxin already far enough downstream to be causing symptoms. As reported in the Annals of Emergency Medicine in 1999, Singer, et al. evaluated 1,171 procedures and reported that NG tube insertion was the most painful. Was the doctor trying to be vengeful or thorough? The old adage, “Doctor, don’t just stand there, do something,” sometimes needs to be replaced with “Doctor, don’t just do something; stand there,” particularly when the therapy is unpleasant and ineffective.
Teaching point: First, do no harm.
Risk management/patient safety issue #4:
Error: Not addressing documented complaints, i.e., syncope and chest pain.
Discussion:
• Question: “Doctor, have you ever seen a case of ___?”
• Answer: “No, I have never seen a one.”
•
Question: “Never seen, or never diagnosed?”
The physician started with a chief complaint of epigastric pain, but after he heard about the bad turkey sandwich, it was all over. The complaints of syncope as documented by the paramedics and chest pain documented by the nurse should throw this differential wide open. Even if the chief complaint was accurately noted to be epigastric pain, there are non-abdominal etiologies that can be responsible for this constellation of symptoms, cardiac ischemia being one of the most serious. An ECG was performed, meaning this diagnosis was considered, but a progress note was not present to explain why the life-threatening diagnosis was not occurring. Additionally, a good history could have easily explored this potentially serious diagnosis with questions about an exertional component, radiation to the shoulder(s) or jaw, associated symptoms of dyspnea or diaphoresis, and of course, risk factors.
Teaching point: A diagnosis not considered is a diagnosis not made.



2 Comments
So, what was the answer…?
The answer is aortic dissection (he may have had undiagnosed marfan’s) — died at age 36.