In writing about medical errors, health policy researcher Robert Wears, MD, breaks down a common problem in how we view mistakes in general. We often choose to view the error or mistake a person makes as a linear process and assign blame to that individual, but it’s rarely that simple. A medical error (or any mistake for that matter) is usually the result of a confluence of many different occurrences. The error or mistake is not the cause, but the result.
Avoid diagnostic errors by taking a moment to ask yourself a few standard questions
 In writing about medical errors, health policy researcher Robert Wears, MD, breaks down a common problem in how we view mistakes in general. We often choose to view the error or mistake a person makes as a linear process and assign blame to that individual, but it’s rarely that simple. A medical error (or any mistake for that matter) is usually the result of a confluence of many different occurrences. The error or mistake is not the cause, but the result.
In writing about medical errors, health policy researcher Robert Wears, MD, breaks down a common problem in how we view mistakes in general. We often choose to view the error or mistake a person makes as a linear process and assign blame to that individual, but it’s rarely that simple. A medical error (or any mistake for that matter) is usually the result of a confluence of many different occurrences. The error or mistake is not the cause, but the result.
The overwhelming majority of our decision making occurs at the unconscious level, based on well developed patterns of recognition that work fast and exceedingly well most of the time. This is how we often know what is wrong quickly, and it does very well until it encounters a new or novel situation for which it has no established pattern. Our conscious mind, the prefrontal cortex, oversees the work of the unconscious, always on the lookout for circumstances which do not exactly match a pattern. Such outliers are few and far between, so staying focused to identify them takes a lot of energy. The prefrontal cortex has very limited capacity, thought capable to only handle four to nine variables at a time, so it is easily overwhelmed. Moreover, it tries to rationalize the available information into a plausable explanation that fits, but may not be real. Your prefrontal cortex is into plausability, not reality.
Correctly diagnosing someone with back pain 99 out of 100 times is quite outstanding. But when we see the IV drug user for the fifth time this month with low back pain as he prances around the room needing something for relief, we can easily decide – first unconsciously and then consciously – to discount his new complaint of leg weakness.
This is hard to overcome, especially when the confluence of these circumstances has us barreling down the track on our way to the presumed diagnostic certainty our unconscious mind has decided. Our prefrontal cortex needs some help, a chance to pause briefly without interruption, even if for a moment, to reflect. Just as Scott Weingart talks about cognitive stops in the mind of the resuscitationist, the diagnostician needs a checklist against their decision making. Pat Croskerry chronicles many of the ways we can be misled and provides some guidance for response in ‘The Importance of Cognitive Errors in Diagnosis and Strategies to Minimize Them’ (Academic Medicine, August 2003). These are helpful resources, but I would like to propose the following structure for “cognitive pauses” during diagnosis.
First Stop:
After initial evaluation, categorize the patient’s issues
a) Straightforward: Few possibilities, all of low risk, path to diagnosis is clear cut, (ie. everyone does it this way.) Think ankle injury
b) Complicated: Few possibilities, but some potentially serious, path to diagnosis is clear cut, (i.e. everyone does it this way) Think chest pain with a description very compatible with ACS
c) Complex: Many possibilities, some potentially dangerous, path to diagnosis is not clear cut, just deciding how to get started takes some thought. Think multiple complaints that don’t fit together, weak and dizzy, abdominal pain
If straightforward, move on and later finish with step 3
If complicated, pause
- Are there any outlier symptoms?
- If none, move on and later, finish with step 3
- If there are, continue to step 2
If complex, definitely continue now to step 2
The purpose of the initial evaluation is to probe deeply for any symptoms that don’t fit. Although a scary proposition, ‘opening the hood’ to hear everything on their mind takes on a new significance; the presence of any outlier symptoms surfaces the need to challenge the plausable explanation.
Second Stop:
After categorizing:
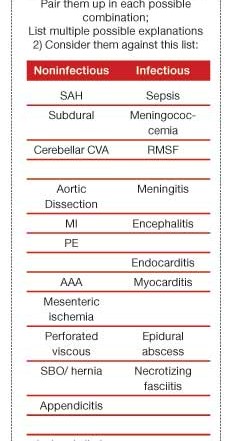
a) Match up the different/outlier symptoms. One definition of innovation is the connection of previously unconnected thoughts/ideas. On paper, pair two of the symptoms at a time in each possible combination. This visual depiction jogs the brain to recognize patterns that might not have been apparent.
b) Check these against a list of can’t-miss diagnoses.
Caring for patients with complex presentations is a creative endeavor. Many disparate facts and perceptions must be compiled, many possible options must be considered, and then a unique path is forged together with the patient. Interestingly, this creativity might actually require that the pre-frontal cortex be turned off. Our day is spent toggling between creativity when categorizing patients, and, once categorized, conformity to the accepted standards. How we do this moment by moment is a fascinating but not well understood process.
Third Stop:
After all the evaluation and review is done and there is a working diagnosis:
a) Why is this not correct?
b) Why can’t this be an embryonic illness (as Greg Henry says, one too early in its course to be diagnosable?)
c) If it might be? What must I do to prepare the patient/family for their role after discharge – to detect that the possible embryonic illness is actually happening
Framing these in the negative challenges the brain to reconsider its plausible explanation by focusing on what does not fit, that element we rationalize for plausability, but whose recognition is the key to avoiding diagnostic error and mistake. Moreover, this might alert us to the possibility that the correct diagnosis can not yet be known, so we must create a plan with the appropriate margin for safety.
Conclusion
The first and third stops are for everyone. Identifying the few patients each shift that require step two early on in their visit reduces the stress on your pre-frontal cortex. Most experienced EPs likely have some similar technique, whether consciously or not. Better understanding this process has profound, valuable implications for training, teaching, oversight of midlevels, and a healthy career.
Once settled into your next shift, give the three steps a try. This cognitive pause only takes seconds. Consider keeping the checklist to the right on your desktop for easy reference. See if it helps you consider diagnoses that might not otherwise come to mind. Better yet, commit your own process to paper and send it in to share. We’d love to see it. Email your thoughts to editor@epmonthly.online