Here’s a formula – and an app – to help you catch this easy-to-miss diagnosis
I have to tell this story from my point of view because I don’t want anyone to think that the recognition of LAD occlusion was made retrospectively. I want everyone to know that, with the right mind preparation and the use of the early repolarization (normal variant ST elevation) vs. LAD occlusion formula, extremely subtle coronary occlusions can be detected, or at least suspected, prospectively — from the ECG alone.
The Case
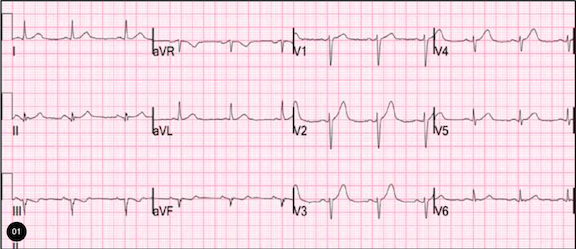
I was reading dozens of leftover ECGs on a weekend and saw this one.

The computerized QTc is 402 ms. There are symmetric T-waves and poor R-wave progression. There is 1 mm of ST elevation at the J-point in leads V2 and V3. This formerly met “criteria” for thrombolytics in the ACC/AHA guidelines of 2004, though, of course, this amount of ST elevation is very nonspecific. It is nonspecific because normal variant ST elevation can be even much greater. However, normal variant ST elevation always has better R-wave progression and typically has asymmetric T-waves that have a slow upstroke and a rapid downstroke (See image 2).

Above is a case of early repolarization. Note the slow upstroke and fast downstroke of the T-wave. It is asymmetric.
So, this was my thinking at this point in the case: If this patient presented to the ED with chest pain, then this is an LAD occlusion. So I went to look at the chart and found this history:
A male in his 40s, with no history of coronary artery disease who had a couple of episodes of chest pain during the day, then presented with one hour of constant substernal chest pain.
This is such a subtle ECG that I was worried that it had gone unnoticed, and, in fact, it did.
His pain continued and his ECG was read as normal. His first troponin was normal. He was admitted to the hospital for “rule out MI.” His second troponin I returned at t = 5 hours and was elevated at 3.8 ng/ml. His ECG was repeated at this point — five hours after the first (see image 3).

Image 3 shows a well developed anterior STEMI, with deep QS-waves (indicating extensive infarction) and persistent ST elevation.
Sometimes normal T-waves are symmetric; however, ST elevation with poor R-wave progression is not normal ST elevation. See this comparison in image 4. On the right is our patient with LAD occlusion. On the left is a patient without anterior ischemia. Notice the T-waves are symmetric in both of them, but the R-wave progression is preserved in the one on the left (and there is less ST elevation). Although these may appear similar at first glance, they are distinctly different.

So, here’s what happened next: The cath lab was activated and an LAD occlusion was found and opened. The peak troponin I was > 100 ng/mL. On echocardiogram, there was a 40% ejection fraction with anterior wall motion abnormality.
I applied the LAD occlusion/early repolarization formula to the first ECG using the “subtleSTEMI” iPhone app [1].
- QTc is the computerized QTc
- RAV4 = R-wave amplitude in lead V4
- STE 60 V3 = ST Elevation at 60 ms after the J-point, in lead V3, relative to the PQ junction
Formula: (1.196 x STE 60 V3) + (0.059 x computerized QTc) – (0.326 x RA V4); a value > 23.4 is quite sensitive and specific for LAD occlusion; > 22.0 is 96% sensitive and 81% specific.
With a QTc of 402ms, STE60V3 of 1.5 mm, and R-wave amplitude in V4 of 3 mm, the result was = 24.5, which is > 23.4 and indicates LAD occlusion; the number is so high because of the very low R-wave amplitude, which in comparing subtle LAD occlusion to early repolarization is the single best predictor of LAD occlusion — better than ST elevation. It is critical to apply this only when the differential diagnosis is early repol (normal variant ST elevation) vs. subtle anterior MI. LVH may cause false positives. See iPhone app and sidebar of blog for instructions.
To not see these findings is very common, and this patient would typically be given an admitting and discharge diagnosis of NonSTEMI.
This is not a missed STEMI; it is a missed coronary occlusion. As you can see, the subtle findings are apparent and, with a prepared mind, can be detected. Studies show that 20-30% of NonSTEMI have an occluded infarct artery at the time of angiography done 24 hours after presentation, and these patients have worse outcomes: higher mortality, more CHF, higher biomarkers, and worse ejection fractions than the NonSTEMI patients with open arteries [3,4,5,6,7]. Indeed, many can be discovered at presentation by recognition of subtle ECG findings.
In addition, this patient had continued to experience ongoing pain, which demands serial ECGs. If there had been serial ECGs, then the evolution of ST elevation would have been detected much earlier and there would be less myocardial injury.
Fesmire et al. showed that, with continuous ST segment monitoring, the sensitivity of the ECG for STEMI rises from 48% to 62% of all MI as diagnosed by CK-MB [2]. In other words, NonSTEMIs are frequently diagnosed as STEMIs if you give them time to evolve.
REFERENCES
1. Smith SW et al. Electrocardiographic Differentiation of Early Repolarization From Subtle Anterior ST-Segment Elevation Myocardial Infarction. Ann Emerg Med 2012;60:45-56. Full text link: http://download.journals.elsevierhealth.com/pdfs/journals/0196-0644/PIIS0196064412001606.pdf
2. Fesmire FM, Percy RF, Bardoner JB, Wharton DR, Calhoun FB. Usefulness of automated serial 12-lead ECG monitoring during the initial emergency department evaluation of patients with chest pain. Ann Emerg Med 1998;31(1):3-11.
3. Wang T, et al. Incidence, distribution, and prognostic impact of occluded culprit arteries among patients with non–ST-elevation acute coronary syndromes undergoing diagnostic angiography Am Heart J 2009;157(4):716-23.
4. From AM, et al. Acute Myocardial Infarction Due to Left Circumflex Artery Occlusion and Significance of ST-Segment Elevation. Amercan Journal of Cardiology 2010;106(8):1081-5.
5. Sorajja P, et al. Impact of delay to angioplasty in patients with acute coronary syndromes undergoing invasive management: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) trial. J Am Coll Cardiol 2010;55(14):1416-24.
6. Pride YB, et al. Angiographic and Clinical Outcomes Among Patients With Acute Coronary Syndromes Presenting With Isolated Anterior ST-Segment Depression: A TRITON–TIMI. Journal of the American College of Cardiology: Cardiovascular Interventions 2010;3(8):806-11.
7. Marti D et al. Incidence Incidence, angiographic features and outcomes of patients presenting with subtle ST-elevation myocardial infarction. Am Heart J December 2014; 168:884-90.



1 Comment
So, in your ED, where you train everyone on these criteria, is this a malpractice event? The patient suffered harm due to misdiagnosis.