Performing a proximal lower extremity ultrasound for DVT.
You’re working a busy emergency department (ED) shift, and the next patient to be picked up on the track board is a 55-year-old man with “leg pain.” You immediately look at the clock and realize that ultrasound has just left for the night and won’t be back until 8 a.m. You say a quick prayer hoping the patient has sprained their ankle.
You go in the room to see the patient, and he has a swollen left leg. He tells you how he recently flew back from Europe after visiting family. He is a smoker. He denies prior trauma. On exam, his entire leg is swollen compared to the right leg. It is tender with pitting edema.
Upon returning to your workstation, you calculate the patients Well’s score and realize he is high risk for deep venous thrombosis (DVT). Unfortunately, because of this you cannot rule out DVT in him with a normal dimer.
Now you have to make the decision between keeping him overnight in the ED for nine hours while he awaits ultrasound, giving him a shot of anticoagulation and relying on him to come back in the morning, or performing your own scan at the bedside.
You grab the ultrasound machine as you decide that a bedside ultrasound will be the most time effective management for the patient. You lay him supine with his left hip slightly externally rotated and abducted. You place the high frequency linear probe just distal to the inguinal ligament and identify his common femoral vein in short axis. Remembering the vein is going to be medial to the artery.

Position the probe just distal to the inguinal ligament with the probe indicator (circle) towards the patients right. Here the common femoral vein, greater saphenous vein and common femoral artery will be seen in transverse/short axis. After compression, slide the probe distal to view the bifurcation of the common femoral vein in to the femoral and deep femoral vein.
Applying gentle compression you notice the vein is not collapsing and the artery is slightly distorting. You see a blood clot within the common femoral vein.

Ultrasound image of a hyperechoic blood clot (*) in the common femoral vein (CFV). The vein sits medial to the artery (A).
You complete the procedure by assessing his femoral, deep femoral and popliteal veins. Once his pain is controlled you discharge the patient with anticoagulation and arrange urgent primary care follow-up.
Pearls and Pitfalls for performing a proximal lower extremity ultrasound for DVT
- Ultrasound of the proximal lower extremity for DVT is a procedure that can be completed rapidly and accurately by emergency physicians at the bedside in patients with suspected DVT.
- The patient should be laid supine with their leg externally rotated and abducted.
- Be sure to image the common femoral vein at the level of the greater saphenous vein, as lack of compressibility of either of these vessels would be concerning for a DVT. Continue scanning down the leg in short axis to identify the femoral vein and deep femoral vein.
- To assess the popliteal vein for compression you want to place the probe in the popliteal fossa. Be sure to evaluate the popliteal vein prior to its trifurcation.
- To assess the popliteal vein for compressibility, position the probe in the popliteal fossa with the vein in transverse orientation. Making sure the vein has not started to trifurcate.
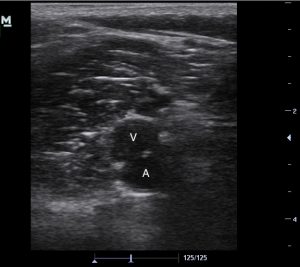
- Transverse ultrasound image of the popliteal vein (V) and artery (A) in the popliteal fossa. The vein sits superficial or posterior to the artery.
- A negative study is when you are able to compress the vein in transverse/short axis and the walls of the vein touch and the lumen completely disappears.
- A positive study is when there is lack of compressibility of the vein and slight distortion of the artery.
- False negatives for this study include compression of superficial veins, compression in long axis orientation, over-compression, and an anechoic thrombus.
- False positives include a Baker’s cyst, inadequate compression, lymph node, abscess and superficial thrombophlebitis.