You are working one evening when EMS brings in a 52-year-old gentleman who achieved return of spontaneous circulation (ROSC) in the field following cardiac arrest. He was walking on his treadmill when he clutched his left shoulder suddenly.
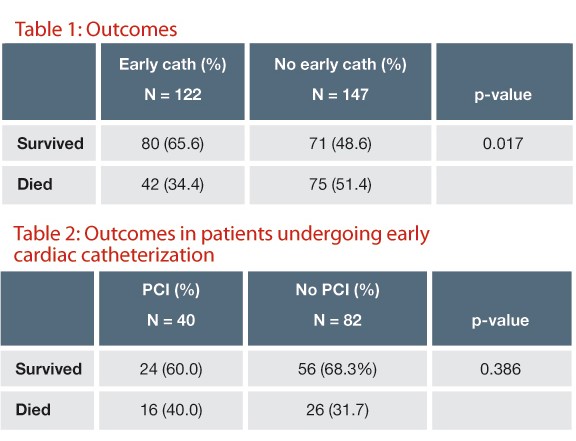
A systematic review analyzing the efficacy of cardiac caths following resuscitation from VT and VF
You are working one evening when EMS brings in a 52-year-old gentleman who achieved return of spontaneous circulation (ROSC) in the field following cardiac arrest. He was walking on his treadmill when he clutched his left shoulder suddenly. He told his wife and daughter he didn’t feel well and then collapsed to the floor. His daughter, a lifeguard, performed chest compressions while his wife called 911. On EMS arrival, the patient was found to be in ventricular fibrillation (VF) and was successfully defibrillated. After ROSC, the patient remained comatose and was intubated en route to the hospital. His arrival ECG reveals ST-depression with T-wave inversions in leads V1-3; no ST-elevation is present. After stabilizing the patient and initiating therapeutic hypothermia, you consider whether this patient should undergo emergent cardiac catheterization.
The Options
- Activate your hospital’s cath lab and call in the interventional cardiologist
- Obtain a cardiology consult in the ED
- Admit the patient to the ICU for ongoing management
The Question
In adult patients with ROSC following out-of-hospital cardiac arrest (OHCA) due to VF or ventricular tachycardia (VT), without ST-segment elevation myocardial infarction (STEMI), does emergent or urgent cardiac catheterization increase survival with good neurologic function?
The Evidence
Hollenbeck RD, McPherson JA, Mooney MR, et al. Early cardiac catheterization is associated with improved survival in comatose survivors of cardiac arrest without STEMI. Resuscitation. 2013 Aug 6. pii: S0300-9572(13)00396-1. doi: 10.1016/j.resuscitation.2013.07.027. [Epub ahead of print]

The Background
Less than one-third of patients with ROSC following OHCA survive to hospital discharge (Sasson 2010), suggesting room for improvement in post-arrest care. The 2010 AHA Guidelines for Post-Cardiac Arrest Care describe therapeutic hypothermia and “treatment of the underlying cause of cardiac arrest” as the primary goals of post-arrest care. Significant coronary obstruction is identified in the majority of survivors of cardiac arrest (Larsen 2012), with acute myocardial infarction (MI) identified as the cause of arrest in 37% to 61% of cases (Spaulding 1997, Anyfantakis 2009, Chelly 2012). The International Liaison Committee on Resuscitation (ILCOR) recommends that reperfusion therapy be attempted in all patients with STEMI following cardiac arrest. In patients without STEMI, ILCOR is less definitive, and recommends only that one “consider immediate coronary angiography in all post-cardiac arrest patients in whom ACS is suspected.”
One systematic review looking at coronary angiography in OHCA (Larsen 2012) included a meta-analysis of 10 studies in which coronary angiography was performed in select patients. This meta-analysis revealed an unadjusted odds ratio for survival of 2.78 (95% CI 1.89-4.10). While this finding suggests improved outcomes with coronary angiography, these studies did not exclude patients with STEMI, with rates ranging from 12-54%. Given the observational nature of these studies, selection bias likely contributed to the observed survival benefit.
In the Parisian healthcare system, all patients successfully resuscitated after OHCA are transported immediately for coronary angiography. Dumas et al identified 435 patients with ROSC following OHCA without an obvious non-cardiac etiology. Among 301 patients without STEMI, 58% had at least one significant coronary stenosis, although only 26% underwent successful percutaneous coronary intervention (PCI). Another Parisian study attempted to identify ECG findings predictive of angiographically-defined acute MI (Sideris 2011). The combination of ST-elevation, ST-depression, left bundle branch block (LBBB), or nonspecific QRS widening had a sensitivity of 100%, a specificity of 47%, a positive predictive value of 52%, and a negative predictive value of 100%. Of 46 patients without ST-elevation who were positive by ECG criteria, only 7 (15%) had angiographically-defined acute MI. While use of this rule would decrease unnecessary cardiac catheterization in the Parisian system, its use in most US institutions would significantly increase cardiac catheterization rates. The benefit of such an increase would need to be verified prior to its implementation in light of the increased cost and risks of the procedure.
The current research is a retrospective study performed using prospectively collected data from the International Cardiac Arrest Registry (INTCAR) from 6 large US tertiary care centers. All patients aged ≥ 18 years who survived to hospital admission following OHCA due to VF or VT, without STEMI, and remained comatose, were eligible for inclusion. All patients received therapeutic hypothermia to a core body temperature of 32-34o C for 24 hours following ROSC. Patients were divided into those who received cardiac catheterization within 24 hours of ROSC, and those who either underwent catheterization more than 24 hours after ROSC or did not undergo catheterization. The primary outcome was survival to hospital discharge; secondary outcomes included survival to discharge with good neurologic function (CPC score of 1 or 2), and survival to follow-up.
Results
Of 754 patients who survived to hospital admission, 435 had VF or VT as the initial documented rhythm. Of these, 269 had no signs of STEMI and were included in the analysis. Of these, 45.3% underwent early catheterization and 54.6% did not. The two groups were similar with respect to mean age (60.4 vs. 59.9 years), rates of bystander CPR (54.6% vs. 59.7%), percent with witnessed arrest (85.3% vs. 85.6%), and mean time to ROSC (22.0 minutes vs. 21.9 minutes). Patients with early catheterization were more likely to be in shock at hospital admission (40.5% vs. 25.7%, p = 0.013), and were more likely to receive aspirin (36.9% vs. 13.6%), antithrombin agents (32.8% vs. 12.9%), and glycoprotein IIb/IIIa inhibitors (9.8% vs. 1.4%).
Overall, 56.5% of patients survived to discharge; more patients in the early catheterization group survived (65.6% vs. 48.6%, p = 0.017) and had good neurologic outcome (60.7% vs. 44.5%, p = 0.017), with an adjusted odds ratio of death of 0.35 (95% CI 0.18-0.70, p = 0.003). Of those receiving early catheterization, 33% underwent successful PCI. Survival rates were similar between those who received PCI and those who did not (60% vs. 68.3%, p = 0.386) as were rates of good neurologic outcome (60% vs. 62.2%, p = 0.669). The median follow-up interval was 5 months for those who received early catheterization and 6 months for those who did not. Survival was higher at follow-up in the early catheterization group (60% vs. 40.4%, p = 0.005), as was survival with good neurologic function (60% vs. 39.7%, p = 0.004).
The Bottom Line
In this retrospective, observational study of comatose patients resuscitated from OHCA due to VF or VT, survival was higher among those who underwent early cardiac catheterization. Surprisingly, successful PCI itself was not associated with improvement in survival rates or neurologic outcomes, suggesting that factors other than catheterization led to the improved outcomes. It is possible that the increased use of other interventions, such as anti-thrombin and antiplatelet agents, may have been responsible. Given the retrospective nature of the study, it seems more likely that selection bias played a role: patients suspected of having a better prognosis may have been referred for catheterization, whereas those in whom aggressive care was felt to be futile would be treated more conservatively. Additionally, important prognostic indicators were not addressed in this study. Baseline characteristics provided were primarily related to the arrest itself (witnessed arrest, bystander CPR, time to ROSC) and did not address prior history of coronary artery disease or the presence of pre-existing comorbidities, such as cancer, that could lead to the implementation of less aggressive care.
While coronary occlusion and acute MI are responsible for a significant proportion of cardiac arrests, even in the absence of ST-elevation, the existing literature provides little direction as to which patients would benefit from cardiac catheterization. The data suggests that patients with conduction defects or ECG changes consistent with ischemia are more likely to have significant coronary obstruction; unfortunately, there is no evidence that performing routine catheterization in these patients improves outcomes. The data also does not currently support routine catheterization in patients with VF or VT, given the methodological limitations in the Hollenbeck paper. Consideration may still be given to selective catheterization in patients with a history concerning for acute MI preceding arrest, especially in the presence of ischemic ECG changes. Further studies will need to prospectively evaluate the use of angiography in a pre-defined subset of patients without STEMI to assess its efficacy.
Dr. Cohn practices emergency medicine at Washington University in St. Louis and is the director of the Washington University EM Journal Club