Performing an ultrasound-guided joint aspiration.
A 52-year-old female presents with left elbow pain beginning about a day ago. She associates swelling and redness, but denies injury, fevers or vomiting. She says she is left-handed and recently started a job stocking shelves at the grocery store. On further review of her history, she tells you she has chronic bronchitis and is frequently on steroids.
Upon examination, she has an erythematous and warm left elbow, without induration. There is swelling concerning for a possible joint effusion and she is unable to move her elbow due to pain.
The patient is given intravenous pain medication and a left elbow x-ray is obtained. The x-ray is negative for fracture, tophi or joint erosions. However, it is concerning for a moderate sized joint effusion.
You re-assess the patient and she is still in a considerable amount of pain and unwilling to range her left elbow. Additional pain medications are given and an ultrasound is performed.
With the patient’s left elbow held in flexion the linear probe is placed on the dorsal aspect of the distal humerus in a vertical orientation.

Positioning of the high frequency linear transducer on the distal humerus. The indicator (red dot) is towards the patient’s head.

Ultrasound image of elbow joint. The triceps tendon (T) is visualized in long axis. The distal humerus (H) is seen at the bottom of the ultrasound screen. It is hyperechoic or bright white with posterior shadowing. A joint effusion (*) sits between the humerus and triceps tendon and appears anechoic or black.
Superficial to the triceps tendon a small amount of edema and cobblestoning is seen. Deep to the triceps tendon and superficial to the humerus an anechoic or black fluid collection is visualized. This is consistent with a moderate sized joint effusion. Based on this finding and the patient’s exam you are concerned for a septic joint.
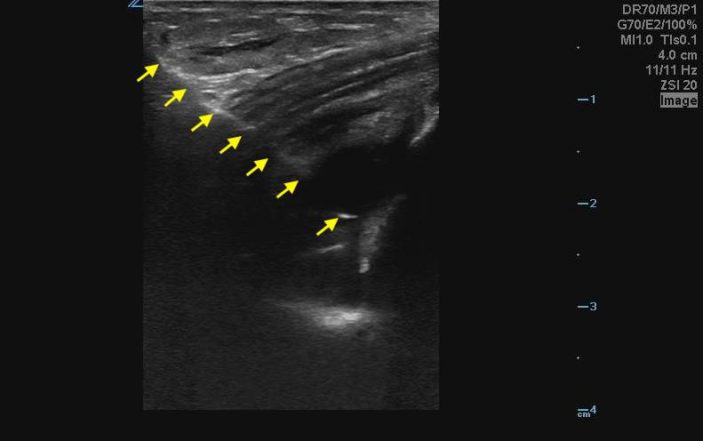
Using a sterile field and making sure you are not over an area of cellulitis; you insert your needle from the superior aspect aiming downward at a 45-degree angle. Using an in-plane approach you are able to follow the needle shaft and tip throughout the entire procedure. Going through the tendon you avoid any nerve or vascular structures and aspirate 15 ml of cloudy joint fluid.

The full length of the needle is seen coursing through subcutaneous tissue, tendon and into the joint space from left to right on the ultrasound screen (yellow arrows). The needle shaft and tip appear hyperechoic. The needle tip is seen within the joint fluid.
A short time later the laboratory calls to confirm your suspicion of a septic joint. You order antibiotics and consult orthopedics.
Pearls and Pitfalls for performing an Ultrasound-Guided Joint Aspiration
- Ultrasound is a great adjunct for joint aspirations as you can see where the joint fluid is located, how big the pocket of fluid is and directly guide your needle into the fluid. Additionally, you can avoid surrounding structures like nerves and blood vessels.
- Using an in-plane approach allows you to visualize the entire length of the needle, its trajectory and know where the needle tip is at all times. This helps to improve success of the procedure and avoid injury to surrounding structures.
- For aspiration of the elbow joint, the high frequency linear probe is used with the indicator towards the patient’s head. The probe is placed on the dorsal aspect of the distal humerus in a vertical orientation.
- This positioning of the probe allows visualization of the triceps tendon and distal humerus in long axis. A joint effusion will be seen tracking between these two anatomic structures and will be anechoic.
- While this case discusses a posterior approach to ultrasound guided joint aspiration using an in-plane technique, it is important to keep in mind there are alternative ways to perform this procedure.
- A lateral joint aspiration can be performed by placing the transducer in a transverse orientation over the radio-capitellar joint.
- Although an in-plane approach is preferred, both an in-plane and out-of-plane approach can be used. When performing an out-of-plane approach be sure to always follow the needle tip to avoid injury to surrounding structures.
References:
Malanga G, Mautner K. Atlas of ultrasound-guided musculoskeletal injections. New York, NY: McGraw Hill; 2014: 52-56.