Core faculty publication requirements have turned some residencies into paper factories. Let’s take a hard look at why we do research, and what truly makes a better resident.
I recently read an article in TIME magazine about the inappropriateness of many scientific medical publications. The article discussed how money is made and careers are enhanced by numbers and locations of articles. There were references to buying authorships on Chinese papers and various other transgressions that made our profession look dirty. This got me thinking about core faculty publication requirements that exist within emergency medicine. Are they really appropriate?
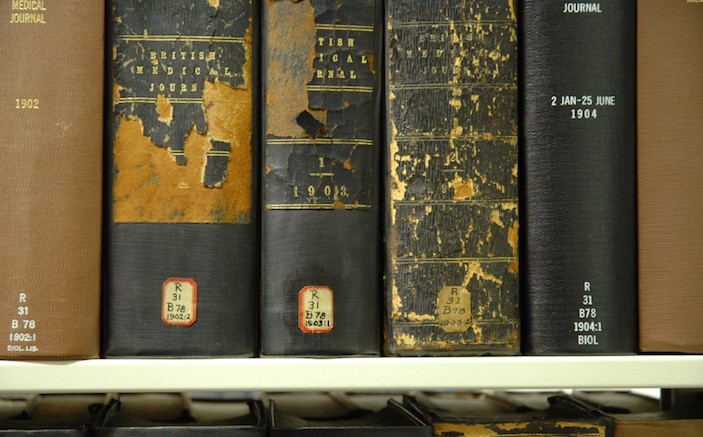
I am core faculty at an osteopathic emergency medicine residency that is applying for ACGME accreditation. One requirement is that core faculty have PubMed identified publications. Now this is a worthy requirement for the nearby University of Michigan with its enormous staff, research assistants, volunteers, students, and bureaucracy. They do great work and I am grateful to have such a fine institution and quaternary hospital backing the rest of us up. But we are a small downtown hospital serving a largely uninsured patient population that cannot afford large monetary outlays for research. We have a strong clinical program and produce good emergency physicians who have successful careers. Asking for double-blind placebo-controlled research is unrealistic and unaffordable. The real quest for small programs like ours is to put something – anything! – in print. With hundreds of thousands of articles published in thousands of journals (yes there really are thousands of scientific journals) do we really need to produce more papers? Of course I can produce a paper and have it published for a fee of just $1,300 or so. But perhaps that is exactly what the TIME article was talking about.
I understand that to become a specialty Ron Krome et al had to bring some body of knowledge to the house of medicine that was emergency medicine’s own. Research was very important in the early years to even have emergency medicine become recognized as a specialty. But, what is the reason everyone must do it now? Its original purpose was not to preclude programs from existing, but it seems to have become exclusionary over time.
Very few graduates will practice in academic centers, so it is hard to contend that they need to be researching or see research being done in order to practice emergency medicine. Surely, the reason to do research now is the same as the reason one might give national level lectures or write chapters in books – to develop and bring expertise into the emergency medicine so that it may evolve and improve. But I am certain that research is not the only way to meet this need. Actually, it is probably not a particularly good way to do it.
Don’t misunderstand me. Research is very important to medicine and to emergency medicine in particular. It cannot and should not be removed from our oeuvre. What I am asking is why does everyone have to do it? Why is it an accreditation requirement? Where is the benefit for our residencies? Where is the evidence that it helps residents be better emergency physicians? Would not the goal of enhancing a residency be as well served (or better served) by lecturing to a national audience or developing an ACEP clinical policy? The participant becomes an expert in the area of concern and brings this expertise to the residency. I’m sure you can imagine many other laudable scholarly activities that would achieve the same goal.
The recent lay press has included articles on bad medical publications and the inappropriateness of ‘publish or perish’. We intrinsically know this is true, but no one seems to want to say it. Our residents need knowledgeable faculty, not people who just make papers. We need to stop this trend toward over-prioritizing faculty publications and seek a better balance. Let us ask that publications be one of many ways that the core faculty can satisfy the scholarly activity requirement for accreditation.



2 Comments
Research publications are not randomized double-blinded placebo-controlled trials or nothing. There is a huge range of possibilities, including interesting case reports that cost only time and effort, survey-based studies or retrospective analyses which are not cost-prohibitive and relatively easily attainable particularly in today’s EMR-laden environments. The fact that most published research originates from centers that treat a higher percentage of lower-income self pay patients casts doubt on the premise of the article. The idea that an entire program could go without some or ample research being performed, denying residents of exposure to the process of pondering questions not asked, thinking outside the box, formulating and conducting studies or writing manuscripts is worrisome and such a trend against promoting research will set our profession back. Many attendings, myself included, only became interested in research because of exposure to it during residency. Academic inbreeding at training programs that do not meet research requirements only further contributes to this problem. To be frank, this lack of research is more of a cultural issue amongst many Osteopathic training programs, one that will need to be rectified in the comings years with the joint ACGME/AACOM/AOA merger. The question raised above of whether research is proven to benefit a resident’s training is an interesting research topic for such a resource-limited training program to study and publish.
The requirement to publish by faculty and residents is one of the reasons most of the medical literature isn’t worth the paper it’s printed on. Albert Einstein observed, “An academic career in which a person is forced to produce scientific writings in great amounts creates a danger of intellectual superficiality.” Because of the academic publish or perish culture we are now drowning in a sea of intellectual superficiality. Thanks Dr. Webley for taking a rational stand on this issue.