Even when completely false, accusations of inappropriate conduct can ruin a physician’s career. Here are five strategies for staying above reproach.
The recent arrest of a prominent emergency physician after accusations of inappropriate behaviors while treating patients in an emergency department have left many of us confused and on edge. Since the only facts of the case are those published in newspapers, we cannot draw any conclusions about the allegations, but must always keep in mind that anyone accused of any crime is presumed innocent until proven guilty. In addition, HIPAA prevents medical providers from publicly disclosing any information about a patient’s medical care or condition without express written permission, thereby prohibiting a public response to allegations of wrongdoing.
Even though our legal system provides every accused citizen with a presumption of innocence, hospital administrators, professional organizations, and the general public are often not so forgiving. The mere accusation of professional wrongdoing can easily wreak havoc on a physician’s career. One need only look through comment sections in newspaper articles about physicians accused of wrongdoing to see that public sentiment often presumes guilt, not innocence. A simple internet search shows multiple examples of physicians whose careers have been ruined by allegations of impropriety (references at the bottom).
Sadly, there are few resources available to help physicians navigate accusations of inappropriate behavior. As we considered how to best discuss this topic, we thought it would be most appropriate to provide readers with some background on the personal and professional repercussions that may occur when an allegation of impropriety is made, how to minimize the chances of patients making such allegations, and some general suggestions on what to do if targeted by allegations of impropriety.
Effects of An Allegation of Impropriety
Perhaps the most immediate impact of an allegation of inappropriate behavior is the healthcare provider’s job security. Institutions put patient rights and concerns foremost and healthcare providers are often immediately removed from patient care duties when an accusation of misconduct is made. Most physician employment agreements contain language permitting the hospital or employer to terminate the physician’s contract for vague reasons, such as if a physician’s actions “are in any way detrimental to the reputation, character, or standing of the hospital or any of its employees” – leaving a physician one negative newspaper article away from losing his or her job. While a physician may ultimately be vindicated from any allegations, by that time the damage will likely be uncorrectable and long-lasting [2].
Professional impact of allegations of impropriety may range from becoming insecure with medical practices and losing confidence in one’s abilities to becoming completely unemployable. Social and reputational stigma may cause the accused physician to become socially isolated which impacts both family life and emotional stability. Financial strain in responding to such accusations may range from using up retirement savings to losing one’s home while attempting to defend against such allegations. Attorneys may be required to defend the physician against both civil and criminal complaints. Insurers may even void coverage for allegations of criminal wrongdoing and those same criminal allegations may result in incarceration.
Professional effects of impropriety don’t end with one’s hospital privileges. State Medical Boards treat allegations of misconduct seriously and place a high priority on investigating any accusations of sexual misconduct. In addition, the Federation of State Medical Boards uses a broad definition of sexual impropriety to include “expressions of thoughts and feelings or gestures that are sexual or that reasonably may be construed by a patient or patient’s surrogate as sexual [3].” Some examples of sexual impropriety listed by the FSMB include “watching a patient dress or undress,” “inappropriate comments about or to patients,” “criticizing a patients’ sexual orientation,” “performing an intimate examination … without explaining the need for such examination,” and “touching breasts, genitals, or any sexualized body part for any purpose other than appropriate examination or treatment.” If a Board investigation determines that there is a “reasonable probability that the physician has engaged in sexual misconduct,” it will “take appropriate action to ensure the protection of the patient and the public at large.” The FSMB also notes that “findings of sexual misconduct are often sufficiently egregious as to warrant revocation of a physician’s medical license.” In other words, a physician is likely to have his or her license suspended if the State Medical Board believes that there is a reasonable possibility of misconduct and is likely to have his or her license revoked if the misconduct is proven. Loss of a physician’s license in one state will be reported to the National Practitioner Databank and will often prompt licensure actions in any other state where the physician is licensed.
Avoiding Accusations of Impropriety
While a basic cornerstone of the physician-patient relationship is trust, the best way of addressing accusations of professional misconduct is to avoid the accusations in the first place. While there is no way to prevent malicious patients from making untrue or exaggerated claims of inappropriate behavior, below are some suggestions from our editors to help minimize settings where patients may perceive inappropriate touching and to help a physician refute untrue claims. We also welcome all comments and suggestions from our readers for additional strategies.
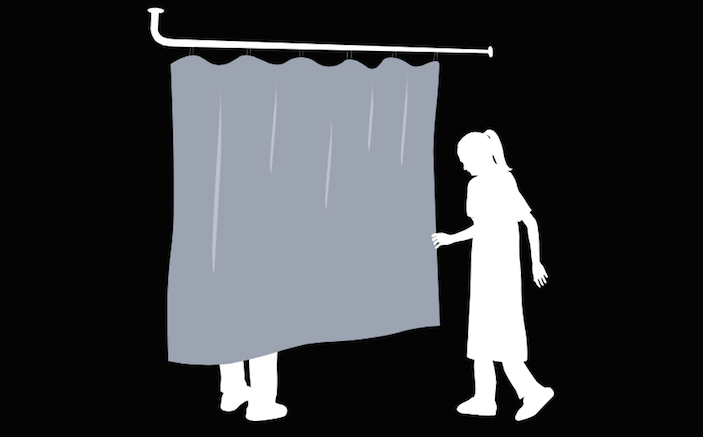
Chaperone chaperone chaperone: Having a chaperone present any time a patient’s personal areas are examined is probably the best defense against accusations of inappropriate touching. In cases where a patient is uneasy about an exam, having two chaperones in the room may be reasonable. Note the names (or initials) of the chaperone in the medical records under the description of your exam. If the chaperone is a nurse, the chaperone should also make a chart entry noting that he or she was present for the exam. In addition, the chaperone should avoid leaving a physician in the room alone with the patient. If the chaperone leaves the room to get necessary supplies, walk out of the room as well and stand in the hallway where either someone can see you or where a security camera can visualize you. If a patient’s family members are waiting in the hallway while you perform your exam, comment to them that you are stepping out of the room to respect the patient’s privacy while the chaperone has left the room.
Privacy but not seclusion: Even with a chaperone in the room, consider pulling curtains to give patients privacy, but also consider leaving the door open an inch or so. By leaving the door open, if anyone in the room calls for help, the voices will be more likely be heard down the hallway. If a patient’s family members are present, asking them to wait outside the door instead of in the waiting room during an exam may provide both the patient and family members with added peace of mind knowing that help is nearby.
Maintain separation: Allowing patients to remain gowned and covered by sheets when discussing the patient’s complaints and history can make patients feel less vulnerable. When performing an examination near any portion of a patient’s genitals (including the female breasts), wearing gloves not only provides a physical barrier to minimize spread of bacteria, but also provides the impression that the physician is being professional and not trying to take advantage of the patient. When palpating a female patient’s chest for pain (such as after a motor vehicle accident), the patient’s hands can be used as a barrier between the physician’s hands and the chest wall. Move the patient’s hands to different areas on the chest wall and then press through the patient’s fingers looking for pain. If necessary, a patient can also be asked to lift her breast tissue with her hand to allow for better auscultation of her heart.
Opt out: Patients who express uneasiness about a physician’s gender or about having an examination of sensitive areas can always opt out of that portion of the examination. If the examination is an important part of evaluating the patient’s presenting complaint, then the patient should ideally sign an informed refusal acknowledging that the physician discussed the risks of refusing this aspect of the exam and that the patient accepts any consequences or delays in diagnosis resulting from such refusal. Discussions of this nature are best made with at least one other witness in the room who can sign the informed refusal.
Follow policies: Hospitals may have policies regarding examination of patients and use of chaperones. It is always a good idea to review departmental or institutional policies to determine whether your actions are in compliance with hospital directives.
What To Do If An Accusation Has Been Made
In most instances, complaints of impropriety can be investigated by the department director or hospital administration and quickly resolved. However, some complaints unfortunately become picked up by the media and quickly spiral out of control. In any case where an accusation of improper behavior may result in further action being taken against the physician, additional responses may be considered.
Many of the issues involving an accusation of impropriety involve legal questions. Probably the best initial step in combatting any allegation of improper professional behavior is to retain an attorney who is well-versed in employment law and health care related matters. Because a physician’s hospital privileges and licensure may be affected, early contact between legal counsel and hospital administration may help preserve the physician’s livelihood. The American Health Lawyers Association or a physician’s specific State Bar Association are two good places to look for attorney referrals. If criminal charges have been filed, it may be necessary to retain a criminal defense attorney as well. By retaining an attorney, any requests for interviews from investigators can be filtered through legal counsel. In high-stakes situations such as these, it is advisable not to discuss the case without an attorney present.
When accusations are published on social media or in the news, it may be tempting to respond to the allegations. Keep in mind that HIPAA prevents disclosure of a patient’s protected health information unless a permissible use under either 45 CFR 164.502 or 45 C.F.R. § 164.512 exists. Responding to allegations of impropriety in the media is not included within HIPAA’s permissible uses of protected health information. In addition, hospital policies often forbid health providers from discussing patient care issues online or in the media. If questioned about accusations online or in the media, the safest response is either no response at all, a simple denial of the allegations, or a referral to the hospital administration or to your attorney for comment. Do not be baited into attacking the accuser or providing unauthorized disclosure of the accuser’s protected health information.
In high-profile cases, it may be worthwhile to consider retaining a public relations consultant to assist in addressing the media barrage. This consultant would be considered a “business associate” under HIPAA and would therefore be subject to the same restrictions on disclosing protected health information as the physician and other covered entities.
Whether or not a formal complaint or a lawsuit has been filed, it would be wise to inform your malpractice carrier about any patient allegations of impropriety. Coverage for many insurance policies is bound when a claim is made or reported. By reporting an incident, not only are physicians able to bind coverage for the alleged event, but they are also able to access any resources the insurance company has available to defend against such accusations. In addition, the insurance company may be able to assign an attorney to assist in the physician’s defense.
Coping with the emotional repercussions from an accusation of professional malfeasance is more difficult. Pressures on an accused physician’s family may benefit from family crisis counseling. The American College of Emergency Physicians has no formal process in place to assist members who are having difficulty with stressful professional issues. The American Academy of Emergency Medicine has an informal process where its members may contact AAEM if the members are in a difficult situation and an AAEM Board Member will typically respond to offer general assistance. AAEM does not offer legal advice. State medical societies may offer referrals for professional counseling services and larger hospital systems may offer in-house peer counseling or wellness services which may help a physician transition through difficult emotional times. Private professional counseling services such as Physician Leadership or MD Mentor can also be considered. There are also hundreds of books available on Amazon about how to cope with physician stress.
Conclusion
Being accused of professional malfeasance often comes as a shock to the physician and can be a life- and career-altering event. Taking steps to minimize the patient’s perception of potential unprofessionalism and to maximize the patient’s privacy may help to decrease the chances of such accusations. If an accusation of impropriety has been made against you, don’t go it alone. Seek guidance to help you with the emotional, professional, and legal impacts that such accusations can cause.
REFERENCES
- www.michigan.gov/documents/mdeh/sexual_boundaries_Between_Patients_and_Healthcare_Provider1_221316_7.pdf. Accessed Feb 12, 2016
- https://www.fsmb.org/Media/Default/PDF/FSMB/Advocacy/GRPOL_Sexual%20Boundaries.pdf. Accessed Feb 12, 2016
- www.ajustnhs.com/case-histories-of-victimised-nhs-staff/ http://www.Stories of NHS Staff/A Better NHS. Accessed Feb 12, 2016









7 Comments
Excellent and timely article. The realization that we are ALL one negative news article away from a malpractice claim, loss of a job, license, insurance coverage and therefore employability, reputation, savings and potentially liberty should hit home, HARD, with every EP.
I do have a question for the authors. HIPAA figures into this so prominently. Although you would of course have privileged communications with your attorney, and patient information is at issue in most such cases, it can be shared confidentially with your attorney. I’m not at all sure that would apply with PR professionals. Wouldn’t they be limited to knowing what has already been published by the patient?
We tend to accept the departments we work in. But design clearly can mitigate risks for both patients and providers.
Well-placed security cameras coverings all hallways and doors to patients rooms, can provide evidence of who was in what room when, how long they were there, and if they were being chaperonnned. A picture is worth a thousand words, and despite what the medical record says, if there is video proof, people tend to back down pretty quickly if evidence does not support the claim.
Curtains with open doors with layout of the department placing each room around a nursing station provides visual privacy while keeping all patients in close auditory proximity to another staff member.
At some point in the 21st century, we have to question why we are documenting visits with 19th century technology (paper charts and pens), or 20th century technology (an EHR via computer). We have hit the point where it is a logistical possibility to start documenting audio and video of each patient interaction. Colonoscopies are videotaped. Why are we not recording all patient interactions as we approach the year 2020.
Right Shoulder pain has always been a difficult workup, till now.
I am sure the painful shoulder is much better.
The recent Atlanta Journal Constitution series brings all of this home again. My comments at https://www.linkedin.com/pulse/article/some-things-i-wish-didnt-learn-md-jd-fifem-md-mentor- or the series itself at http://doctors.ajc.com/sex_abuse_national_database/?ecmp=doctorssexabuse_microsite_stories
The advice in the article above about specific behaviors to avoid is worth re-reading. Another important issue is ALWAYS to wear gloves when touching any part of a patient that could be considered erogenous, including mouth and genitals. Breasts are in a “grey zone”, but unless you are doing a real exam (not just checking for obvious pathology such as a huge breast mass) it makes sense to palpate over a gown. If looking for discharge, etc. of course you should wear gloves. And a chaperone could document that you are wearing them.
Something that is not mentioned in the article but that becomes apparent in the series is that a “curbstone consult” is in many states illegal, and in all states inadvisable. If no record is kept, most states would consider this an impermissible practice of medicine on a colleague or family member. Add to this the potential for allegations of misconduct by an employee and you have a recipe for disaster.
I recently had a total right hip replacement. After an innocent misunderstanding with a nurse about having INADVERTENTLY caught her changing trash bags across the room from my own on my new kindle while trying to figure out how to take a selfie of me I my room ,Almost instantly, things got heated, and she took my kindle to “help” me delete the pic that was apparently one my kindle ” cloud” as well. When I got the device back almost an hour later, having gone looking for her, and it, t had shown signs of being opened, and not even closed completely. As soon as I complained to PVP of patient care and crisis, I was accused of asking a nurse to get into bed with me,on multiple occasions,that had supposedly been witnessed by no fear than four others. Sorry for the long story, but I ‘m getting no names dates circumstances, or anything. I’d now had nine major surgeries, and this is a first. I’ furious, INNOCENT, and want answers. I had asked the hospital to replace the $100.00 Kindle my wife bought me before the surgery,as ever the home page had been altered, along with who knows what else. Then the false sexual allegations.
The facility has been great to me in the past, Had to be readmitted three days after initial release to monitor severe leg pain redness and possible blood clot. Had that happen in 2005 for acl/xml repair as well. Where do I go from here, without ruining people’s careers?
I know i am late to the party but i think it to be Then creditly necessary and even more so important to state that first i will say i am so very sorry that you were put in such unprofessional misconduct by a hospital persoanel but also accused of such horrendous acts; while literally trying to mind your own business and recover.
Now just in case anyone else reads this & knows better than to make the mistake that this poor bloke did. These people here on this page arent at all here to assist & help the patients. These guys are the ones who help the accused; The bad guys for lack of better words.
With that being stated yes its true that we have crazy ,mean, down right cruel people in this world that are willing to accuse someone of misconduct when truth be told there was nothing of the sort. We have to admit that we have more serial rapist, child molesters, sexual deviant people that come from all walks of life. So i love all the good advice as to the best taken approach is to have a buddy system in lamen terms but lets state facts here. I am one year away from tuning 50 years of age. Everything that was stated in this article is #1 taught in school. If for any reasons it wasnt there is a HUGE problem. I am a victim that didnt speak up. Physicians taking advantage of their patients coping little weird & extremly unnecessary exams have been going on for far too long. People who try to help those accused by trying to blame the victims should be ashamed of themselves. This is the reason as to why i never spoke up. It hasnt just happened to me once; ive experienced this type of behaviour on multiple occasions. I guess i am just the unlucky one. I think not. I am almost certain that just as priest, boy scouts leaders & many others in these trusting roles come out the more serious, the more real we as a society will now take that we have a problem. We have a huge problem that may or have caused people a lifetime of depression, pain, unhealthy, unhappy lives has been swpet under the rug for far too long.
Look at this man who asked a question about his situation & no one, not a single person gave him advice ? Why?? My guess is because he is a patient. You dare believe that your colleges just happens to be a sexual preditor, why??
Face the facts folks its real more than its not. Most physicians get away with it. Most times we are afraid to say something. We do not think that anyone will listen, we think that we have no rjghts. Its a shame really. You guys know that all doctors know to take a nurse, family member or staff in that room with them. Thats been a rule for a very long time . Last thing i would now like to add is that i am a nursing graduate but after graduating i decided to not continue a career in nursing. After having many issues with these sexual illicit, sexual deviant physicians that i have been unforrunate to meet. I am not saying all physicians but i am saying that probably 1 in every 20 physicians have some issues. At least thats been my Experience. To finish this very long reply that ive written. I must add that thru my own personal experience if it isnt thru their touching Inappropriately, or by Not having someone else in the room ( even after being asked ), Making extreme inappropriate comments and jokes that many physicians cross the line, in my Opinion and experience. Some tend to play very close to even getting caughr. Almost like a game to them. I hope that as we progress we will have to deal with that type of Behavior less & less. Truth be told we as a society need to learn to not side with someone bc we are colleges or bc we think we know that person. We need to learn to stay neutral. We never know sometimes we are working, living, standing, tallking next, with, around a monster. Remember it doesnt make us wrong or bad for not knowing but before you so quickly defend without knowing the facts or unless you were there you do not know. This is facts!!!
Agree 100%!!!
Yes we are now in 2022 video Technology has Progressed So rapidly it’s mind blowing!!! I think it Can steer On a Negative reaction When we are talking about caring for a patient And conducting Exams That are of such a sensitive nature. Lets be honest no one wants to have their pap smear recorded. This would just feel not only Unnatural but extremely uncomfortable. Where would such sensitive recordings be kept? How could we be completely certain that a Computer hacker or due to a burglary that such sensitive video get into the wrong hands. Of course these are just some of what the negative consequences could result behind having such Sensitive and personal videos. Idk the answers all i do know is that doctors offices seems to show the most common place of concerns due to their being privately owned & ran. Employess afraid to lose thier jobs if they were to speak up.